 Osteoporosis is a term that describes the loss of calcium from bones resulting in bones that are thin. Since parathyroid hormone (PTH) removes calcium from bones (that is what it does), all patients with a parathyroid problem will eventually develop thin bones. Bones with osteoporosis due to parathyroid problems can ache and hurt because the PTH is actively destroying the bone. Bones with osteoporosis are fragile bones which are much more susceptible to fractures and breaks.
Osteoporosis is a term that describes the loss of calcium from bones resulting in bones that are thin. Since parathyroid hormone (PTH) removes calcium from bones (that is what it does), all patients with a parathyroid problem will eventually develop thin bones. Bones with osteoporosis due to parathyroid problems can ache and hurt because the PTH is actively destroying the bone. Bones with osteoporosis are fragile bones which are much more susceptible to fractures and breaks.
Calcium is what makes our bones hard and strong. The calcium level in all parts of our bodies (including the amount of calcium in our bones) is regulated by the parathyroid glands. That's all the parathyroid glands do--regulate calcium throughout the body. Through the secretion of parathyroid hormone (PTH), these four small parathyroid glands regulate how much calcium is absorbed from our diet, how much calcium is released into the urine by our kidneys, how much calcium is contained within our nervous system and muscles, and how much calcium is stored in our bones. We store many pounds of calcium in our bones, and nearly all of this calcium is readily available to the rest of the body at the request of the parathyroid glands. When one (or more) of the parathyroid glands are overactive (hyperparathyroidism), our bones release calcium constantly into the blood stream. It is the excess parathyroid hormone that is causing this! The result of too much parathyroid hormone is that bones lose their density and hardness. If that wasn't bad enough, the excess calcium removed from the bones stays in your blood making you feel bad (see our page on symptoms). If you have kidney stones and hyperparathyroidism--guess where the kidney stones came from? That's right, the calcium in the kidney stones came from your bones!
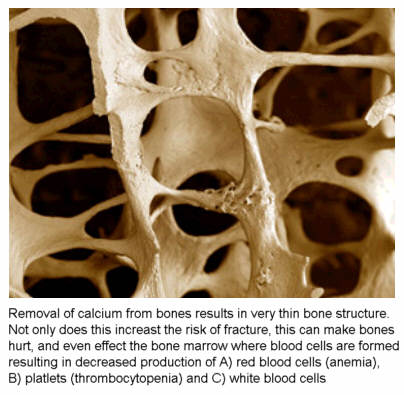
The loss of calcium from bones is called osteoporosis. Bones which have lost some of their calcium are said to be "osteoporotic". Osteoporotic bones are more likely to break. In fact, the definition of osteoporosis indicates that the likelihood of fracture is 10 times higher than normal. Yep, a 10-fold increase in the incidence of fracture. If you have severe osteoporosis, the risk of fracture increases up to 25-fold! The picture of the yellow bones above and to the right a bit shows a normal bone section on the bottom and a bone with osteoporosis on the top. The osteoporotic bone has bigger holes in it as a result of the calcium being dissolved and put into the blood stream. Osteoporosis has 3 causes: 1) excess parathyroid hormone, 2) advanced age, and 3) lack of estrogen in older females. This page is primarily about cause number one--osteoporosis due to parathyroid disease...although you can see that if you are a female over the age of 50 you are getting a triple-whammy.
 Osteoporotic bone is not as strong as regular bone and therefore, bones that have osteoporosis are much more susceptible to fractures. All patients with hyperparathyroidism will get osteoporosis if the parathyroid tumor is not removed...even young patients. This continued dissolving of the central bone is what causes the bone pain so common to hyperparathyroidism. It is also what contributes to the weakening of the spinal column resulting in elderly persons walking "hunched over". The picture on the right shows what a normal bone (left) and an osteoporotic bone (right) look like under a microscope. You can see that the bone on the right is much less dense and has more open areas. There is much less calcium structure that gives the bone its strength. The process of losing the calcium out of the bones is often felt as an aching pain in the bones (hips, legs, wrists, and lower back usually).
Osteoporotic bone is not as strong as regular bone and therefore, bones that have osteoporosis are much more susceptible to fractures. All patients with hyperparathyroidism will get osteoporosis if the parathyroid tumor is not removed...even young patients. This continued dissolving of the central bone is what causes the bone pain so common to hyperparathyroidism. It is also what contributes to the weakening of the spinal column resulting in elderly persons walking "hunched over". The picture on the right shows what a normal bone (left) and an osteoporotic bone (right) look like under a microscope. You can see that the bone on the right is much less dense and has more open areas. There is much less calcium structure that gives the bone its strength. The process of losing the calcium out of the bones is often felt as an aching pain in the bones (hips, legs, wrists, and lower back usually).
 Osteoporosis is seen very nicely in this picture. This is an actual photo of a broken hip bone from a man with osteoporosis due to a parathyroid tumor. The osteoporosis is seen as bone that is very thin. It actually looks weak and you can imaging how this bone is more prone to break than a normal bone that is thick and strong. Patients with parathyroid tumors will get osteoporosis that is more severe than people without parathyroid tumors, and the osteoporosis develops faster than osteoporosis which is not associated with a parathyroid tumor. Remember, the drugs which have been developed for the treatment of osteoporosis (Fosamax, Actonel, Evista, Boniva, Miacalcin, etc,) are very good drugs for routine osteoporosis, but they were not designed to work in patients with parathyroid tumors, and they do not. Let us say this again, taking Fosamax or Actonel (or any other osteoporosis medicine) will not help the osteoporosis in a man or woman who has a parathyroid tumor. If your calcium and/or PTH is high, then you almost certainly have a parathyroid tumor that needs to be removed so this process can be stopped (and reversed in most cases).
Osteoporosis is seen very nicely in this picture. This is an actual photo of a broken hip bone from a man with osteoporosis due to a parathyroid tumor. The osteoporosis is seen as bone that is very thin. It actually looks weak and you can imaging how this bone is more prone to break than a normal bone that is thick and strong. Patients with parathyroid tumors will get osteoporosis that is more severe than people without parathyroid tumors, and the osteoporosis develops faster than osteoporosis which is not associated with a parathyroid tumor. Remember, the drugs which have been developed for the treatment of osteoporosis (Fosamax, Actonel, Evista, Boniva, Miacalcin, etc,) are very good drugs for routine osteoporosis, but they were not designed to work in patients with parathyroid tumors, and they do not. Let us say this again, taking Fosamax or Actonel (or any other osteoporosis medicine) will not help the osteoporosis in a man or woman who has a parathyroid tumor. If your calcium and/or PTH is high, then you almost certainly have a parathyroid tumor that needs to be removed so this process can be stopped (and reversed in most cases).
 The picture of the skeleton on the left shows in different colors where osteoporosis occurs most commonly and therefore, where people with osteoporosis are most likely to break a bone. Note that the lower back, the hips, and the wrist are the most common places to break a bone if you have osteoporosis. The loss of bone density in the lower 1/2 of the spine is why people get shorter if they have osteoporosis. If you don't address it, then you can end up bent over...because the vertebrae of the lower back get crushed on the front part making it seem as if the person is bent over. The test that is done to check the density of bones is called a "DEXA" scan. When you get a DEXA scan you will see that they check two main areas... the lower 4 lumbar vertebrae, and several areas of the hip. Now you know why.
The picture of the skeleton on the left shows in different colors where osteoporosis occurs most commonly and therefore, where people with osteoporosis are most likely to break a bone. Note that the lower back, the hips, and the wrist are the most common places to break a bone if you have osteoporosis. The loss of bone density in the lower 1/2 of the spine is why people get shorter if they have osteoporosis. If you don't address it, then you can end up bent over...because the vertebrae of the lower back get crushed on the front part making it seem as if the person is bent over. The test that is done to check the density of bones is called a "DEXA" scan. When you get a DEXA scan you will see that they check two main areas... the lower 4 lumbar vertebrae, and several areas of the hip. Now you know why.
Our bones are at their strongest in our early 20's. They stay at this level of strength for a number of years, but then begin to lose strength slowly when we are in our mid 30's. Once we hit mid-life, we all lose a little bone density, but this is most evident for women. Estrogens have a protective effect on bone density which becomes evident after menopause when women begin to lose calcium from their bones at a faster rate then men of the same age. That is one of the reasons most doctors feel that most post-menopausal women should be on some form of estrogen therapy. If you are a woman then you probably know this is a little controversial, but the reason that estrogens are even considered is to protect the bones from the normal (slow) loss of bones. HOWEVER, if you have a problem with a parathyroid gland (hyperparathyroidism), the osteoporosis is EXTREMELY ACCELERATED. As you will learn later on this page, there is no medication for osteoporosis associated with hyperparathyroidism. Estrogens will NOT help and will not slow down the process if you have a parathyroid problem. Actonel, Evista, Fosamax, Boniva, Miacalcin, Reclast, etc, etc, will NOT help if you have a parathyroid problem. The parathyroid problem MUST be addressed. Please watch a 6-minute video of Dr Norman discussing this concept. This is a very popular and award-winning video.
 As you know from other pages of this web site, overactive parathyroid glands secrete too much parathyroid hormone. The excess parathyroid hormone (PTH) has a direct effect on the bones... this is how parathyroid hormone is supposed to work... except that it's out of control when people have hyperparathyroidism. The excess PTH secreted from the parathyroid tumor causes calcium to leave the bones and go into the blood. The bones become osteoporotic and prone to fractures. The problem is amplified greatly in post-menopausal women since this process is ongoing already! This can also be a big problem for people of all ages if it goes on for several years, making the bones weaker year after year.
As you know from other pages of this web site, overactive parathyroid glands secrete too much parathyroid hormone. The excess parathyroid hormone (PTH) has a direct effect on the bones... this is how parathyroid hormone is supposed to work... except that it's out of control when people have hyperparathyroidism. The excess PTH secreted from the parathyroid tumor causes calcium to leave the bones and go into the blood. The bones become osteoporotic and prone to fractures. The problem is amplified greatly in post-menopausal women since this process is ongoing already! This can also be a big problem for people of all ages if it goes on for several years, making the bones weaker year after year.
The picture on the right is a famous picture of a sea-captain who had parathyroid disease that was not treated and it destroyed his body. It was his disease that allowed doctors to better understand the function of the parathyroid glands and the problems with ignoring a parathyroid tumor. His name was Captain Charles Martel. The picture on the left is Captain Martel in his early 30's, and on the right he is shown at the age of 50. Captain Martel had terrible osteoporosis because of a parathyroid tumor that was not diagnosed. This bad osteoporosis caused him to shrink and become very ill with the other problems caused by the high calcium in his blood (which came from the bones!), like bad heart disease. These photos of Captain Martel were taken in the 1920's at the time when we were figuring out that the parathyroid tumor in his neck produced too much hormone and the hormone was eating away at his bones. This is about the same time when the hormone "insulin" was being discovered as a cause of diabetes. The point here is that all patients with hyperparathyroidism (a parathyroid tumor) will get osteoporosis, and it can be very severe osteoporosis.
- All patients with hyperparathyroid disease will develop osteoporosis- regardless of their age or sex! Let us say that again... ALL patients will get osteoporosis regardless of age if they don't get their parathyroid tumor removed.
- Women tend to develop osteoporosis from parathyroid disease faster than men.
- Post-menopausal women with parathyroid disease will generally develop osteoporosis 2-5 times faster than their peers.
- The osteoporosis associated with parathyroid disease is often extreme. The most extreme (worst) osteoporosis is seen in patients with untreated hyperparathyroidism.
- Men and women in their 30's and 40's can develop osteoporosis due to parathyroid over-activity.
- Teenagers and people in their 20's can have osteoporosis if they have a parathyroid tumor.
- About 70% of all patients with parathyroid disease will already have osteoporosis when their doctor finally figures out they have hyperparathyroidism. Thus, ALL patients with hyperparathyroidism should have a DEXA scan as soon as the diagnosis of hyperparathyroidism is made.
- Osteoporosis due to parathyroid disease can often cause bone pain and joint pain. Removing the bad parathyroid gland usually fixes this completely. Interestingly, this pain is usually gone within 6 to 12 hours after the parathyroid tumor is removed. Often, this is very dramatic!
- There is NO MEDICINE that can stop the worsening of osteoporosis due to parathyroid disease. It will continue to get worse even if you take Fosamax, Actonel, Evista, Boniva, Reclast (etc)... The bones will not stay the same, they will continue to lose calcium and the osteoporosis will get worse. Period.
- Once the parathyroid tumor is removed, virtually 100% of patients will have a significant (and often dramatic) increase in bone density. Osteoporosis associated with hyperparathyroidism is the ONLY type of osteoporosis that is completely reversible!
- Severe osteoporosis is associated with decreased life expectancy for several reasons, but one primary reason is due to the increased risk of severe fractures and their complications.
- One of the reasons people with un-treated parathyroid disease (for more than 10 years) have a shorter life expectancy is because of the bad osteoporosis--the calcium in the bones is gone and much of it is deposited in the arteries, causing bad atherosclerosis (hardening of the arteries).
- We have another quick page you need to read... it shows that life insurance companies know that hyperparathyroidism will decrease your life expectancy and may not insure you if you don't get it fixed BEFORE you get osteoporosis. Click Here to read.
Will Fixing the Overactive Parathyroids Help the Osteoporosis?
 YES! YES! YES!
YES! YES! YES!
It has been known for many years that removing the bad parathyroid gland (or glands) (and the excess parathyroid hormone it produces) will stop the rapid and continuous loss of bone density. What was not known was whether the body would try to restore the calcium levels in the bones. Several recent studies have shown that the body will restore bone density after the excess hormone is removed. Researchers at the University of Northern Sweden studied the bone density of postmenopausal women (average age 63) with primary hyperparathyroidism before and one year after parathyroidectomy [Thorsen, et al, Surgery 1997;122:882-7]. They found a significant increase in bone density in the hip and lower back one year later. This is a very slow process, and the bones will take many years to repair themselves, it does not happen overnight. In fact, depending on how much bone density has been lost, they may never regain their "normal" calcium levels and overall density. But at least we know that parathyroidectomy doesn't just stop the rapid loss of bone density, it allows the body to begin healing itself.
updated (Editorial note from Dr. Norman: After taking care of many thousands of patients with significant osteoporosis due to parathyroid disease, It is my opinion that nearly all of these patients will begin to re-gain bone density following a successful parathyroid operation. Nearly all will show increased bone density in the first year which will continue for at least 4 years. Another huge advantage is that these patients often have bone pain and joint pain ... which will be relieved almost immediately after a successful parathyroid operation in about 90-95% of patients. Most claim their bone pain is completely gone. The best part is that bone pain usually goes away within 2-3 hours after the operation!).
Can I Do Anything to Help Increase Bone Density and Decrease the Amount of Osteoporosis?
This is written for patients with hyperparathyroidism. And the answer is "nobody knows for sure, but we think so". All experts are now recommending that most patients take supplemental calcium AFTER an operation to cure their hyperparathyroidism. IMPORTANTLY>>> If you have hyperparathyroidism you CAN NOT take calcium pills when the tumor is still in your neck! It will make your calcium go higher and increase your risk of having a stroke! If your calcium is high, you can NOT take calcium pills!!! AFTER the parathyroid tumor is out, you should take calcium pills every day-this will increase your bone density and decrease (and even alleviate) your osteoporosis. How long should you be on calcium pills AFTER your parathyroid operation?? It depends on your age, sex, menopausal status, and if you have a documented loss of bone density. The following list reflects most endocrinologists' and endocrine surgeons' overall feelings regarding who should take supplemental calcium, but it is NOT written in stone, and your doctor may feel differently. Take the advice of your doctor in this regard.
- Post-menopausal women
- Anyone with a bone density more than 1 standard deviation below their age-matched peers
- Most patients over the age of 60, male or female
- Young women who are thinking of having children (once pregnant, this MUST be under the care of the obstetrician).
- Dr. Norman recommends that all of his patients take calcium daily for at least one year following parathyroid surgery. For women above the age of 40, he recommends they take two calcium pills daily forever. HOWEVER, Dr Norman also expects all of his patients to have a DEXA scan, that way the dose of calcium pills to be taken daily can be more accurately determined as well as how long they should be taken. REMEMBER... if you have hyperparathyroidism you CANNOT take calcium pills until after the parathyroid tumor has been removed. This is a common mistake--and taking calcium pills when you have a parathyroid problem will not help your bones and instead it will make you feel worse and increase your chances of having a stroke. Do not take calcium pills if you have a parathyroid tumor in your neck!
There are some new drugs available which MAY help increase bone density even faster, but only after the bad parathyroid gland has been removed. These drugs are specifically designed to make bones add calcium to their structure. They have not been studied scientifically in the setting of hyperparathyroidism. In fact, it is a bad idea to take drugs such as Fosamax, Actonel, Evista, Boniva, and Reclast as an alternative to parathyroid surgery. None of these drugs has EVER been shown to help in patients with parathyroid disease, and the makers of these drugs do not recommend them for this purpose. Similarly, the use of Fosamax and/or Actonel (or any of the rest of these drugs) for the treatment of osteoporosis due to parathyroid disease is NOT an FDA approved use of these drugs. MANY people are put on these medications, but they have never been shown to help...UNTIL the parathyroid gland has been removed. Dr Norman has collected data (soon to be published) of 3500 parathyroid patients who have osteopenia or osteoporosis and who were on Fosamax or Actonel for at least 1 year. The results show: 2% of patients had improvements in bone density, 12% had the same bone density for 1 year, but only 4% had the same bone density for 2 years. 88% of patients had worsening of their bone density, with 63% having severe worsening of the bone density. Thus, these drugs have NO effect on osteoporosis in patients who have a parathyroid tumor. The tumor must be removed before the bones can be made better.
How to read your Bone Density DEXA Scan.
If you have hyperparathyroidism then you must know what your bone density is so you can see how much damage has been done to your bones by the parathyroid tumor, and so you can compare your bone density scores after your parathyroid tumor has been removed so you can see your bones get better every year. Here is the universal bone density scale that is used world wide (adopted by the World health Organization).
Bone density measures give a statistical measure of how good or bad your bones are when compared to people with good bones (in their twenties). There is an average density for young adults and this density is given the score of 0 (zero). Some people will have bones that are a little more dense or a little less dense than average, so therefore it is normal to have a bone density between +1 to -1. If you have lost calcium from your bones then your bone density will go down and your score goes more negative. When your bone density it is -2.5 or higher (in any area of your bones), then you have osteoporosis. The middle ground between -1 and -2.5 is called "osteopenia".This is thin bones, but not quite osteoporosis. It is important for you to understand that osteoporosis in ANY area of your bones means you have osteoporosis. If you have osteoporosis just in the Ward's area of the hip and the rest of the hip and spine have osteopenia... then you have osteoporosis. You either have osteoporosis, or you do not. ANY area that shows a score of -2.5 or more means you have osteoporosis. This is a very common mistake. Do not look at "global" scores (L1 - L4) as this will always underestimate the amount of osteoporosis present.
A good quality DEXA scan should have readings for your lumbar spine and at least one hip. You should have individual measures from both of these areas. If you only have "global" measures of the spine (L1 - L4) then your scan is inadequate and needs to be re-done. This will underestimate the amount of bone loss and should never be done (it is done because it is easier and quicker... and nobody is watching the hen house). A good quality DEXA scan will have at least 10 measures of bone density (the best scans have 20 or more individual readings). The worst have only two. As we said earlier, if you have only two measures of bone density (a global hip and global spine), then the study is not very good and should be repeated.
What to read next
- Read our second (quick) page on osteoporosis due to parathyroid disease and how life insurance companies can use this excuse to not provide you life insurance. They know this little tumor is not good.
- Click here to see a few photos of parathyroid tumors that were removed from people's necks. These pictures show the parathyroid tumor that is making all the parathyroid hormone that is removing all of the calcium out of the bones.
- Watch a video of Dr Norman performing a Mini-Parathyroid operation. Our number one video.
- Take a Video Tour of our new Parathyroid Center and meet our passionate people.
- How to become our patient
This page was last updated: 11/06/2021