High Calcium and Parathyroid Tumor Screening at Hospital Emergency Rooms

Screening for High Calcium, Parathyroid Tumors, and Other Endocrine Tumors Begins at HCA Hospital Emergency Rooms
In Association with the Norman Parathyroid Center and the Hospital for Endocrine Surgery
Endocrine tumors (tumors arising in the adrenal gland, parathyroid glands, and thyroid gland) occur with enough frequency that they can be found in many patients who go to an emergency room for some other reason. Unfortunately, world-wide the healthcare system is not really designed to find these unsuspected endocrine tumors. Thus, the patient being treated for a urinary tract infection who is noted to have high blood calcium, typically has the infection treated and the high calcium glossed over and nothing happens. The patient doesn't know, and the patient's doctor is never told.
Typically, if the patient comes in with belly pain, the workup and diagnosis is centered upon this problem, and the opportunity to find other problems like high calcium, a parathyroid tumor, a thyroid cancer, or an adrenal mass is missed. The purpose of the endocrine screening program is to find endocrine tumors many years sooner than they would otherwise be found. This could affect 100,000 people in the US annually, finding their parathyroid, adrenal or thyroid tumor years sooner providing huge benefits to quality of life and life expectancy for these patients.
Screening for Parathyroid, Adrenal, and Thyroid Tumors in the Emergency Room
This article provides the scientific basis for looking for endocrine tumors for all patients who come into hospital emergency rooms. Other articles will go into more detail about adrenal tumors and thyroid nodules/cancers, with this article having a heavy emphasis on screening for high blood calcium (and therefore, hyperparathyroidism).
When physicians look for a disease in a population of patients it is called "screening". Some forms of tumor screening are well known. Mammograms performed on all women over 40-45 years old is a well known screening program to detect breast cancer while it is still small. Colonoscopy at age 50 is another way that doctors use "screening" to look for a colon cancer that may or may be present. We can do this same type of screening for endocrine tumors without the patient having to do anything--we do it when they come to an emergency room.
Endocrine tumors and the diseases they cause are unique in all of medicine in that they are often identified on routine lab tests or x-rays scans. More specifically, endocrine tumors are routinely identified on scans and blood tests performed on patients seeking emergency care for an unrelated complaint, injury, or illness. The fact that most endocrine tumors show up on routine scans and blood work performed in an emergency room means these tumors are perfect for a screening program. The patient comes to the ER for "problem x" and while he/she is there he gets a scan and some blood work that shows "endocrine tumor Z" --something that nobody was looking for--but it showed up because that's what endocrine tumors do.
It sounds so simple, yet as straightforward and obvious as this is, no screening program for adrenal, thyroid, or parathyroid disease or tumors has ever been undertaken before. It is very unfortunate that more than 50% of patients being operated on for an endocrine tumor such as a parathyroid tumor had evidence of the tumor for more than 8 years on previous blood work or x-ray or CT scan. The tumor was present and yet most doctors ignored it because that was not what the patient was being seen for. This is the problem the new endocrine tumor screening program was designed to fix.
Screening for Parathyroid Tumors and High Blood Calcium in Hospital Emergency Rooms
Finding high blood calcium indicating primary hyperparathyroidism in emergency room patients
Primary Hyperparathyroidism is a disease of the parathyroid glands which causes dramatic abnormalities in calcium metabolism resulting in a cascade of secondary complications, signs and symptoms. Although humans (and all mammals) have four parathyroid glands, the disease is caused by a benign, single adenoma in 80-85% of cases, with enlargement of two or more parathyroid glands in 15-20%. The best epidemiological studies of hyperparathyroidism are via extensive health-screening examinations, mainly from Scandinavia, and consistently demonstrates a prevalence of up to 2.1 % in postmenopausal women (1), and 0.73 % in men (2). The prevalence of hyperparathyroidism in younger individuals is substantially lower. Studies from the Norman Parathyroid Center in over 20,000 patients shows similar rates of 2.0% in women over 50, and 0.7% of men over 50 (3,4) Smaller studies in the United Sates from e.g. the Kaiser Permanente system corroborates these findings (5).
Most People Aren't Aware that High Blood Calcium is Bad
It is estimated that at least 50-60% of patients with primary hyperparathyroidism do not know they have the disease because their serum calcium has not been measured or an elevation in the calcium has not been appreciated for its significance. In a landmark publication in JAMA in 2019 performed through the Veterans Affairs Hospitals in the US, 371,370 veterans (three hundred, seventy one thousand!) where known to have significant hypercalcemia during a 15 year period, yet only 86,887 (23.4%) were evaluated for primary hyperparathyroidism with the measurement of a serum parathyroid hormone level (6). Worse yet, of those, only 6049 (12.8%) of those diagnosed underwent definitive treatment with parathyroidectomy. Like all previous reports, the VA recognizes that “untreated primary hyperparathyroidism impairs quality of life and incurs substantial costs” downstream with dramatic over-utilization of resources, higher mean numbers of medications, more frequent doctor and hospital visits, and increased rates of development of several cancers (breast, prostate, colon, kidney).
It is estimated that approximately 50,000 to 75,000 patients per year that are undiagnosed in the US. Given the prevalence of hyperparathyroidism in large epidemiological studies, it is likely that these numbers are extraordinarily conservative. Every day we have patients share their disappointment in their doctors for not recognizing their high blood calcium years earlier.
ER Screening for High Blood Calcium and Therefore: Hyperparathyroidism
Serum calcium measurements are performed in the vast majority of patients visiting an ER, and thus represent a significant opportunity for case detection and diagnosis, leading to faster and better treatment of these patients who would otherwise have a failure or delay in diagnosis. Given the significant number of serum calcium measurements performed at HCA Emergency Departments, a systemic, comprehensive quality improvement program to identify and diagnose patients became a reality in June 2021 with collaboration and expertise provided by Dr Jim Norman and the other parathyroid experts at the Norman Parathyroid Center.
We selected the trigger age for elevated serum calcium level at age 30 since it is quite rare below this level, and because teenagers have higher levels of calcium than adults. If possible, any patient presenting with a kidney stone should be included regardless of age. The trigger level for the height of serum calcium can be set at any elevated level, however some patients within the emergency room are ill and have not eaten so they may be dehydrated giving a false positive hypercalcemia. However, if the trigger is set to 11.0 mg/dl or higher, this can be expected to provide a positive predictive value of >95%, thereby eliminating the unnecessary workup of individuals who are unlikely to have pHPT. Once experience and data has been collected on enough individuals, this level may be appropriately adjusted down slightly.
A note to our patients and everybody that knows that adults are not supposed to have blood calcium levels over 10.0 mg/dl (2.5 pg/ml). Please understand that we are not trying to find ALL cases of hyperparathyroidism. We are screening for the obvious cases that have been present for years that nobody has diagnosed and caught. If we set the trigger at 10.0 mg/dl then 20% of the adults in the ER would meet this criteria because they are sick, have vomited, and all their electrolytes are out of wack. We are starting at 11.0 which means that over 95% of people we find (and we find about 2 per day per hospital) will be a true positive, not a false test, and therefore we don't overwhelm our endocrinologists with cases that are not correct. We expect this trigger number to come down to 10.5 sometime in the future. But yes, we know that adults over 40 should have virtually all calcium levels in the 9's, and not the 10's. Calcium levels between 10.0 and 11.0 are NOT normal and should ALWAYS be looked into... but for this Emergency Room Screening Program, we can't have lots of sick people vomiting getting confused with the parathyroid patients. This is a fantastic start, and huge progress for parathyroid patients everywhere.
How Does the High Calcium Screening Program Work?
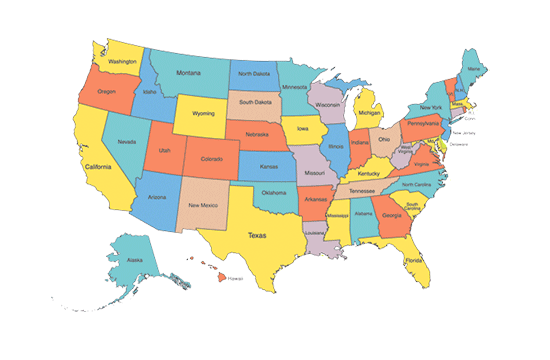
HCA Healthcare, the largest hospital company in the US, with 196 hospitals in 21 states has invested heavily in the endocrine disease field beginning in 2020. In 2021 they built a new hospital in Tampa, Florida dedicated to endocrine tumors: the Hospital for Endocrine Surgery. In keeping with this commitment to improving the diagnosis and treatment of endocrine tumors, HCA worked with Drs Jim Norman, Gary Clayman, and Tobias Carling to adapt their award winning "Care Assure" screening program for lung tumors and heart rhythm problems so it could be used to detect endocrine tumors.
Since nearly all adults going to an emergency room will have their blood drawn for serum electrolytes, the HCA team developed software to examine all calcium levels for adults over 30. Since calcium level above 10.2 mg/dl in person over 30 is usually not normal, and for those over 40 a value above 10.0 mg/dl is usually not normal, that was our starting point. But, many people in the have not been feeling well for hours, or even a day or two, and thus many of them are a little dehydrated and this can cause the measured calcium to be a little higher than it would be if the patient was feeling normal at home.
Thus, we chose a blood calcium level of 11.0 mg/dl or higher as the "trigger" value to identify hypercalcemia (high blood calcium). Patients who are found to have a calcium level of 11.0 mg/dl or higher have a parathyroid tumor about 90% of the time--even with just one blood test. The HCA Care Assure team is comprised of a nurse at every participating hospital who is notified when a patient "triggers" one of the parameters suggesting an endocrine tumor (calcium above 11.0; adrenal tumor on CT scan of 1cm or larger (1/2 inch), or a thyroid nodule larger than 1.5 cm (3/4 inch). The day after the patient is seen in the ER, the nurse contacts the patient to explain the findings, then contacts their primary care doctor. The nurse then sets up an appointment with an endocrinologist to help confirm the diagnosis with further testing. It is up to the primary care doctor and the endocrinologist to determine the course of action, if any, that should be followed. The surgeons at the Hospital for Endocrine Surgery do not play any role in this process. If surgery is needed, the endocrinologist is free to send the patient to a surgeon of their choice.
The Diagnosis of Primary Hyperparathyroidism
The diagnosis of primary hyperparathyroidism is straightforward in almost all cases. Most often the hypercalcemia is identified in patients with multiple non-specific complaints which have long been referred to as “moans and groans”, including depression, chronic fatigue, poorly controlled hypertension, frequent headaches, and many other symptoms. In 25%, hypercalcemia is the cause of kidney stones which left untreated causes kidney failure and nephrocalcinosis. Osteoporosis is common and expected, with fractures of long bones, pelvis and lower spine expected in the vast majority of patients if the disease is untreated.
Elevated serum calcium is the hallmark of primary hyperparathyroidism and therefore seen commonly in patients seeking care in emergency rooms world wide ... about 2% of the adult women in any given emergency room should have it! The workup is straightforward and simple with the elevated serum calcium level needing to be confirmed only once in the vast majority of cases. Intact serum PTH levels should be obtained in all patients with consistently elevated or high-normal serum calcium levels. An elevated PTH or a level in the upper normal range confirms the diagnosis. You can read more about the diagnosis of primary hyperparathyroidism at two very well known pages of Parathyroid.com: Hyperparathyroidism Diagnosis Basics / Hyperparathyroidism Diagnosis Advanced (award-winning page).
How Common are Endocrine Tumors?
- Adrenal: An adrenal "incidentaloma" is defined as a clinically unapparent adrenal mass greater than 1 cm in diameter detected during imaging performed for reasons other than for suspected adrenal disease. in other words, a patient had a CT scan for some other reason and the scan showed an adrenal mass or tumor. Adrenal incidentalomas occur in 3% of the population and 4.5% patients older than 55 years of age.
- Parathyroid: As noted above, hyperparathyroidism due to a parathyroid tumor occurs in one in 50 women in their lifetime (2% risk), and one in 200 men (0.5% risk). It is estimated that 75% of people walking around with high blood calcium and hyperparathyroidism don't know they have it because no doctor has ever gotten excited about the high calcium. This is simply terrible and what the screening program is trying to address.
- Thyroid: Thyroid nodules are common occurring in 15% of adult women (one in 6.6) and 2% of men. The vast majority of these should be biopsied to make sure they are not cancer. We discuss screening for thyroid cancer in emergency rooms on a different blog.
Screening for Endocrine Tumors Requires Doctor and Surgeon Expertise
On March, 2021 the Endocrine Tumor Screening Program was begun at 19 hospitals on the west coast of Florida, expanding to 50 hospitals throughout Florida in the summer of 2021, and then to the southeast US, and eventually nationwide. To get this huge program underway HCA hospitals (the nation's largest hospital system with about 200 hospitals) asked the doctors at the new Hospital for Endocrine Surgery to help out. The expert endocrine surgeons there are by far the most experienced endocrine surgeons in the world, and are affiliated with the:
- Norman Parathyroid Center
- Clayman Thyroid Center
- Suh Scarless Robotic Thyroid Center
- Carling Adrenal Center
The purpose of the endocrine screening program these groups started was to find endocrine tumors many years sooner than they would otherwise be found. Endocrine tumors cause significant morbidity and mortality. That is, they make people feel miserable and often lead to death. Endocrine glands are those that produce hormones, and thus, tumors of endocrine glands (thyroid, parathyroid, adrenal) will often cause many symptoms due to excessive hormone production from the tumor. This happens for 100% of parathyroid tumors, and about 15% of adrenal tumors and thyroid tumors.
Endocrine tumors can also be cancer. Thyroid cancer is the most common--virtually every adult will know somebody with thyroid cancer. Adrenal cancer is uncommon, only seen in a small percent of adrenal tumors. Unfortunately, adrenal cancer can be a very serious cancer.
You can read more about the HCA Endocrine Screening Program at the Screening Page of the Hospital for Endocrine Surgery website.
- Become our patient
- Get the 5-Star rated Calcium-Pro parathyroid diagnosis app
- More about the Norman Parathyroid Center
- More about the Hospital for Endocrine Surgery
References
- Lundgren E, Rastad J, Thrufjell E, Akerström G, Ljunghall S. Population-based screening for primary hyperparathyroidism with serum calcium and parathyroid hormone values in menopausal women. Surgery. 1997 Mar;121(3):287-94. PMID: 9092129.
- Siilin H, Lundgren E, Mallmin H, Mellström D, Ohlsson C, Karlsson M, Orwoll E, Ljunggren O. Prevalence of primary hyperparathyroidism and impact on bone mineral density in elderly men: MrOs Sweden. World J Surg. 2011 Jun;35(6):1266-72. doi: 10.1007/s00268-011-1062-2. PMID: 21445668.
- Boone D, Politz D, Lopez J, Mitchell J, Parrack K, Norman J. Concentration of serum calcium is not correlated with symptoms or severity of primary hyperparathyroidism: An examination of 20,081 consecutive adults. Surgery 2017 Jan;161(1):98-106.doi: 10.1016/j.surg.2016.09.012.
- Norman J, Goodman A, Politz D. Calcium, parathyroid hormone, and vitamin D in patients with primary hyperparathyroidism: normograms developed from 10,000 cases. Endocr Pract. May-Jun 2011;17(3):384-94.doi: 10.4158/EP09346.OR.
- Assadipour Y, Zhou H, Kuo EJ, Haigh PI, Adams AL, Yeh MW. End-organ effects of primary hyperparathyroidism: A population-based study. Surgery. 2019 Jan;165(1):99-104. PMID: 30420089.
- Elizabeth A. Alore, MD, MPH; James W. Suliburk, MD; David J. Ramsey, PhD. Diagnosis and Management of Primary Hyperparathyroidism Across the Veterans Affairs Health Care System. JAMA Intern Med. 2019;179(9):1220-1227. doi:10.1001 Link: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2737917?appId=scweb