Mini-parathyroid surgery has become the preferred way to treat parathyroid disease. This is the second page on mini-parathyroid surgery--discussing how MIRP mini parathyroid surgery is performed. MIRP mini surgery is also called "radioguided parathyroid surgery", as discussed below. There are four keys to mini parathyroid surgery: 1) The surgeon should have a good idea which parathyroid gland is bad before operating (a positive scan is NOT required), 2) the surgeon should know with near 100% accuracy where the parathyroid tumor(s) is NOT located, 3) the surgeon uses a special probe in the operating room that can tell the difference between a parathyroid gland that is making lots of parathyroid hormone (PTH) and which glands are asleep (not making any PTH), and 4), the surgeon can measure how much hormone each of the parathyroid glands are making during the operation. Importantly, the standard parathyroid operation does not do either of these last two important steps, rather the old way simply requires the surgeon to dissect all parts of the neck and "explore" for the parathyroids, hoping to find one that is big so it can be removed. The probe can tell the difference between a normal parathyroid gland and a diseased gland, so normal glands are not removed... and the surgeon knows when the patient is cured by removing a parathyroid tumor that is making LOTS of hormone. The probe tells the surgeon when the bad gland has been removed, and it prevents the removal of normal glands. Look folks, the days of "exploring" people's necks for parathyroid glands are gone. If your surgeon uses the word "explore", then get up and walk out.
Mini-parathyroid surgery has become the preferred way to treat parathyroid disease. This is the second page on mini-parathyroid surgery--discussing how MIRP mini parathyroid surgery is performed. MIRP mini surgery is also called "radioguided parathyroid surgery", as discussed below. There are four keys to mini parathyroid surgery: 1) The surgeon should have a good idea which parathyroid gland is bad before operating (a positive scan is NOT required), 2) the surgeon should know with near 100% accuracy where the parathyroid tumor(s) is NOT located, 3) the surgeon uses a special probe in the operating room that can tell the difference between a parathyroid gland that is making lots of parathyroid hormone (PTH) and which glands are asleep (not making any PTH), and 4), the surgeon can measure how much hormone each of the parathyroid glands are making during the operation. Importantly, the standard parathyroid operation does not do either of these last two important steps, rather the old way simply requires the surgeon to dissect all parts of the neck and "explore" for the parathyroids, hoping to find one that is big so it can be removed. The probe can tell the difference between a normal parathyroid gland and a diseased gland, so normal glands are not removed... and the surgeon knows when the patient is cured by removing a parathyroid tumor that is making LOTS of hormone. The probe tells the surgeon when the bad gland has been removed, and it prevents the removal of normal glands. Look folks, the days of "exploring" people's necks for parathyroid glands are gone. If your surgeon uses the word "explore", then get up and walk out.
Also, if your surgeon wants to operate and take out the gland that shows up on the scan and then quit the operation without checking the other glands then you may want to think about finding a more experienced surgeon (watch our operation video so you understand why it is best check all the other glands). If your surgeon is going to remove the one parathyroid that shows on the scan and then "measure the hormone in your blood to see if it goes down by 50%", then understand that you have a 25% chance of needing a second operation some time down the road. That is what less experienced surgeons do since it is the simple thing. Heck, your gynecologist can operate to remove the parathyroid tumor that shows on your scan--it doesn't take an expert to do that! HOWEVER, if that is all they are going to do, discuss with them what the plan will be if you are not cured. Who will perform the second parathyroid operation, and how much more dangerous will it be the second time. The "fall in 50%" rule is a silly rule that doesn't work very well. Just ask them and see what kind of reaction you get.
As developed by Dr James Norman (at the University of South Florida in Tampa) in the early 1990's, the radioguided mini approach to the parathyroid gland has now been shown to 1) have the highest cure rate of all parathyroid operations, 2) have the lowest complication rate of all parathyroid operations, 3) require the smallest incision and least amount of dissection, 4) is able to be performed under "Light Anesthesia" where almost all patients are not intubated, 5) cost significantly less than other parathyroid operations, 6) require the least amount of time in the hospital of all parathyroid surgeries (about 1.5 hours post-op typically), and 6) has a lower complication rate compared to a standard parathyroid operation.
NOTE: All patients are candidates for a mini-parathyroid surgery. In other words, all patients should discuss mini-parathyroid surgery with their surgeon to see if this option is possible. Also note that a few expert surgeons can perform mini parathyroid surgery on ALL patients, regardless of scan results, and regardless of the presence of co-existing thyroid disease (we perform mini surgery on all patients regardless of scan results). If your doctor cannot give you a 95% guarantee that your operation will be a mini-operation, then you may want to go somewhere else. If your doctor says you can't have a mini-operation because your scan is negative, you really should go somewhere else. Mini surgery can be done on 100% of patients if your surgeon knows how to do it. Mini surgery does NOT require a positive parathyroid scan.
IMPORTANT... Ask your surgeon if he/she is going to evaluate all four parathyroid glands. This is what you want. If your surgeon is going to remove one gland--the bad gland they see on the scan--and then stop the operation, you have a 15% chance of needing another operation in the next year, and an additional 10% chance of needing a second operation in the next 10 years. Be careful of surgeons who say they can do a mini parathyroid operation because you have a positive scan, and their plan is to take out the one bad gland they see on a scan and quit the operation. About 20% of ALL the operations we perform every week are on people who had this mini, one-side parathyroid surgery. Although Dr Norman is one of the "inventors" of one-side parathyroid surgery in the mid 1990's, he does NOT do this one-side operation any more. The failure rate is too high. Watch the video of a 13 minute MIRP parathyroid operation where all four parathyroid glands are examined and TWO tumors are removed--even though the scan only showed only ONE tumor. Between 25 and 30% of people have more than one tumor.
How Minimally Invasive Parathyroid (MIRP) Surgery Works
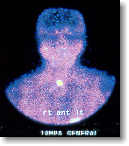 Step 1. Make the over active parathyroid gland radioactive so it can be
differentiated from all the other structures in the neck. The key to the success of
this technique was the development of the Sestamibi scan in the early 1990's which makes
only parathyroid tumors radioactive for about 3-4 hours...normal parathyroid glands will NOT become radioactive (normal glands are asleep, and thus they don't absorb the radioactive dye). This simple technique requires the patient to be given a very small dose of the same drug that is used to examine the heart during heart stress tests. Using special techniques, the bad parathyroid gland will show itself to the surgeon. The surgeon should still look at all four glands if you expect a cure rate over 90%. If your surgeon does not have the expertise to look at all four glands, then he/she will look at only the gland that shows up on the scan. This is fine, however, you must understand that the failure rate will be higher. Ten or fifteen percent of these patients will require another operation because they are not cured.
Step 1. Make the over active parathyroid gland radioactive so it can be
differentiated from all the other structures in the neck. The key to the success of
this technique was the development of the Sestamibi scan in the early 1990's which makes
only parathyroid tumors radioactive for about 3-4 hours...normal parathyroid glands will NOT become radioactive (normal glands are asleep, and thus they don't absorb the radioactive dye). This simple technique requires the patient to be given a very small dose of the same drug that is used to examine the heart during heart stress tests. Using special techniques, the bad parathyroid gland will show itself to the surgeon. The surgeon should still look at all four glands if you expect a cure rate over 90%. If your surgeon does not have the expertise to look at all four glands, then he/she will look at only the gland that shows up on the scan. This is fine, however, you must understand that the failure rate will be higher. Ten or fifteen percent of these patients will require another operation because they are not cured.
 Step 2. Operate to see all four parathyroid glands, but operate only where necessary. The most important information seen on the sestamibi scan is not where the tumor is located, but where the tumor is NOT located. Knowing where the tumors are not located allows an experienced surgeon to see all four parathyroid glands (located where they are supposed to be located) to make sure a second, (or rarely a third) tumor is not present. Now that the surgeon knows that the operation will not require extensive "exploration" of the neck, he/she can make a much smaller incision. The picture on the left shows the incision in the lower neck which is typically made for the minimal parathyroid operation (MIRP). The patient's head is to the top of the picture and a blue pen was used to mark the outline of her collar bones and the top of her breast bone (the sternum). REMEMBER, the old-fashioned standard operation requires a neck incision 4 to 6 inches in length (click here to see a picture of the old parathyroid incision).
Step 2. Operate to see all four parathyroid glands, but operate only where necessary. The most important information seen on the sestamibi scan is not where the tumor is located, but where the tumor is NOT located. Knowing where the tumors are not located allows an experienced surgeon to see all four parathyroid glands (located where they are supposed to be located) to make sure a second, (or rarely a third) tumor is not present. Now that the surgeon knows that the operation will not require extensive "exploration" of the neck, he/she can make a much smaller incision. The picture on the left shows the incision in the lower neck which is typically made for the minimal parathyroid operation (MIRP). The patient's head is to the top of the picture and a blue pen was used to mark the outline of her collar bones and the top of her breast bone (the sternum). REMEMBER, the old-fashioned standard operation requires a neck incision 4 to 6 inches in length (click here to see a picture of the old parathyroid incision).
 Step 3. Use a miniature hand-held radiation detecting probe to measure the amount of activity of each parathyroid gland. The really neat thing about this procedure is that the parathyroid tumor is radioactive for about 3-4 hours...so the surgeon can use this to determine good parathyroid glands (they are asleep and making no hormone) from bad parathyroid glands (they are making too much hormone). The probe measures the amount of radioactivity in each parathyroid gland which is proportional to the amount of hormone being produced. The probe shown here is made by US Surgical Corporation (Norwalk, CT) and was designed and patented by Dr Norman. Since the radioactivity only lasts 3-4 hours, the operation needs to be completed during this period of time. The old way of operating and dissecting throughout the entire neck of all patients with parathyroid disease is giving way to this much improved minimal parathyroid operation for ALL patients. Note... this lets the surgeon know when a gland is normal so it doesn't get removed, and makes sure that ALL of the bad glands are removed--so the patient doesn't need a second operation some months or years later. And, YES, an experienced parathyroid surgeon can see all four parathyroid glands using an incision that is 1 inch or less (slightly bigger in patients over 250 pounds). Our video explains this better
Step 3. Use a miniature hand-held radiation detecting probe to measure the amount of activity of each parathyroid gland. The really neat thing about this procedure is that the parathyroid tumor is radioactive for about 3-4 hours...so the surgeon can use this to determine good parathyroid glands (they are asleep and making no hormone) from bad parathyroid glands (they are making too much hormone). The probe measures the amount of radioactivity in each parathyroid gland which is proportional to the amount of hormone being produced. The probe shown here is made by US Surgical Corporation (Norwalk, CT) and was designed and patented by Dr Norman. Since the radioactivity only lasts 3-4 hours, the operation needs to be completed during this period of time. The old way of operating and dissecting throughout the entire neck of all patients with parathyroid disease is giving way to this much improved minimal parathyroid operation for ALL patients. Note... this lets the surgeon know when a gland is normal so it doesn't get removed, and makes sure that ALL of the bad glands are removed--so the patient doesn't need a second operation some months or years later. And, YES, an experienced parathyroid surgeon can see all four parathyroid glands using an incision that is 1 inch or less (slightly bigger in patients over 250 pounds). Our video explains this better
 Step 4. Remove the radioactive parathyroid tumor. The next step is for the surgeon to dissect the overactive parathyroid tumor away from the rest of the neck structures and remove it. In this picture we put yellow dots around the parathyroid tumor to make it easier to see. This overactive parathyroid was about the size of a large black olive which is fairly typical. Remember, a normal parathyroid gland is supposed to be the size of a pea or grain of rice. Parathyroid glands only have a single small artery and vein. This picture shows a very small clip being put on the artery and vein prior to removing the enlarged parathyroid. If you haven't seen our page of pictures of parathyroid tumors that were removed from patient's necks, you need to see that page soon... Click Here to see pictures.
Step 4. Remove the radioactive parathyroid tumor. The next step is for the surgeon to dissect the overactive parathyroid tumor away from the rest of the neck structures and remove it. In this picture we put yellow dots around the parathyroid tumor to make it easier to see. This overactive parathyroid was about the size of a large black olive which is fairly typical. Remember, a normal parathyroid gland is supposed to be the size of a pea or grain of rice. Parathyroid glands only have a single small artery and vein. This picture shows a very small clip being put on the artery and vein prior to removing the enlarged parathyroid. If you haven't seen our page of pictures of parathyroid tumors that were removed from patient's necks, you need to see that page soon... Click Here to see pictures.
Step 5. Measure the radioactivity in the parathyroid tumor to help make sure that the patient is cured of their disease. The most important aspect of radioguided parathyroid surgery is one that most surgeons who have not been trained in this technique miss (and it has us very frustrated!). The probe is not used to help find the tumor, it is used to determine how much hormone the tumor (or ANY parathyroid gland) is producing. Since the object of the operation is to remove the source of excess parathyroid hormone production, the probe can be used to determine the difference between an adenoma, a hyperplastic parathyroid gland, and a normal parathyroid gland.... Once the enlarged parathyroid gland is out, the probe is placed on it to make sure that the radioactive tumor has been removed. The amount of radioactivity contained within the gland helps the surgeon be confident that the operation is complete and whether or not any other parathyroid glands will need to be dissected out... or even removed. Performed correctly, this method is much more accurate than measuring PTH levels during the operation (over 99% accuracy).
 Step 6. Put on the bandage and get ready to go home. Because the MIRP mini-parathyroid operation can usually be performed quickly with very limited dissection, patients are quite ready to go home within an hour or two. That is fine and they can return to normal duties as soon as they wish (usually the next day). The bandage should be kept dry for about 24 hours, then the patient can shower and do anything they want. The bandage should be left in place about a week. No laboratory tests are required for about 2 months. Of course, this and all of the other decisions and treatments discussed on this page will be up to your doctors...the key is to treat every patient like an individual...each has a special case and special needs. Your case may be different depending on MANY variables, so discuss all of this in detail with your surgeon and work with him/her so you get what is best for YOU.
Step 6. Put on the bandage and get ready to go home. Because the MIRP mini-parathyroid operation can usually be performed quickly with very limited dissection, patients are quite ready to go home within an hour or two. That is fine and they can return to normal duties as soon as they wish (usually the next day). The bandage should be kept dry for about 24 hours, then the patient can shower and do anything they want. The bandage should be left in place about a week. No laboratory tests are required for about 2 months. Of course, this and all of the other decisions and treatments discussed on this page will be up to your doctors...the key is to treat every patient like an individual...each has a special case and special needs. Your case may be different depending on MANY variables, so discuss all of this in detail with your surgeon and work with him/her so you get what is best for YOU.
Why The Experts Are No Longer Performing One-Side Parathyroid Surgery.
Prior to 1993, all parathyroid surgery was performed by the surgeon looking at all four parathyroid glands, meaning that the operation was on both sides of the neck. Without some of the modern tools and hormone measuring devices that we have now, this was a HUGE operation taking 4-6 hours. By 1994 things switched to a one-side parathyroid operation for people with positive scans because of work done by Dr Norman and others who advocated taking out the tumor that showed up on the scan and measuring hormones to predict if the patient was cured--avoiding operating on both sides of the neck. So, between 1995 and 2010, most surgeons would operate on one side of the neck, remove the tumor that was seen on the scan, and then measure the parathyroid hormone to see if the amount of hormone in the blood decreased by a substantial amount. If it did, the operation was concluded. Most surgeons continue to do this now, and it is what these surgeons advertise on the Internet as "Mini Parathyroid Surgery".
HOWEVER, when we look back at what happened to all those patients that we operated on only ONE side of their neck, we see that a lot of these people had to come back and have a second operation because they had a second tumor in their neck that was not removed during the first operation (because the first operation did not look at all four parathyroid glands). Remember, Dr Norman was the biggest advocate of unilateral (one-side) parathyroid surgery for the past 15 years, and is the "father" of mini-parathyroid surgery (Wikipedia). However, Dr Norman and his surgeons stopped doing one-side parathyroid surgery in 2008 because the failure rate was too high. People who had a large parathyroid tumor identified on a scan, and then had this large parathyroid tumor removed by us in the operating room--we expected to be cured. But slowly they started coming back for a second operation. This was in contrast to the people who had a negative scan and we looked at all four of their parathyroid glands during the operation. The people who had negative scans had operations that took about 3 minutes longer, but they were virtually all cured forever because we evaluated all four of their glands, while those with a positive scan had a 12% chance of needing a second operation in the next 10 years. Remember, these failure rates happened to us at our skill level--we're by far the best at this in the world. Even with our experience we can't be sure we cure people forever unless we examine all four parathyroid glands. Thus, if you come to our center, unless certain circumstances exist, we will look at all four of your parathyroid glands, and we will look you in the eye when it is over and tell you about each of them, and how much hormone each of your 4 glands is making. Please watch the video and you will understand this better--we do the same operation on people with positive scans and negative scans, because the only way to cure somebody long-term (for many years) is to look at all four glands in almost all patients. Yes, it is still done with the same small incision, but now you know why our small incisions are always in the middle of the neck--so we can see the parathyroid glands on both sides.
This graph shows what happened to 17,500 patients that we operated on between 1994 and 2010. The vertical axis is the cure rate. The red line shows the people that had a positive scan and we operated on one side of the neck only. The blue line shows people that we operated on both sides of the neck and examined all four parathyroid glands (because the scan was negative, or for a number of other reasons).
It turns out, if we operated on you between 1994 and 2010 and we looked at all four of your parathyroid glands, we never saw you again...you were cured and you stayed cured. You are on the blue line. If we operated on one side of your neck to remove the tumor and didn't examine the glands on the other side of the neck to see if there was a second, smaller tumor, we had a 10% chance of seeing you again in the next ten years to operate on the other side of your neck. We love our patients, but this isn't a good reason to see them twice! Now you know why we look at all four parathyroid glands on about 98% of the operations we do. Because we are smarter now, and we want to cure you (and make you feel better!) for ever, not for just a few months or weeks. Remember, the down side for the patient isn't just that they need a second operation, it is that they never feel as good as they should. They continue to get worsening osteoporosis, fatigue, stones, etc.
Now that we've done this operation over 18,000 times, it takes us only about 17 minutes on average to do a 4-gland operation, and this includes people with thyroid problems. If there are no thyroid problems, the operation usually is about 15-16 minutes. Did you watch the video?
One final note: We can't operate on every patient with this problem. About 8,000 different people view this website EVERY DAY, and they are not all coming to Tampa for surgery! Most of you are going to be operated on by surgeons with little or modest experience with parathyroid surgery. These surgeons are going to do the one-side operation. It is easier for them, and it is safer for you if they aren't doing at least one of these operations per week. Heck, 80-85% of the time this will turn out just fine. If a surgeon doesn't do parathyroid surgery at least once per week, then they are better off only operating on one side of your neck. And, it makes it easier for an expert to re-operate if the first surgeon is unsuccessful. HOWEVER, you must realize that after your operation, your calcium should be in the 9's, not the 10's. If your calcium level is still above 10.0 mg/dl, then you still have a parathyroid tumor in your neck and the one-side operation did not cure you. Be smart folks. Pick your surgeon wisely. Ask good questions. And do NOT let a negative scan keep you from getting your tumor removed. Scans do not matter!
The typical MIRP operation at the Norman Parathyroid Clinic: (Updated: 11/14/2015)
- On average, takes 17.8 minutes (including the patients with thyroid problems) (watch the video of a 13 minute operation.
- Has a cure rate a little over 99% (99.46% for the past 17,500 patients)
- Has a potential complication rate of far less than 1% (near zero in the past 16,000 operations)
- Is performed through a 3/4 inch to 1-inch incision (slightly larger if over 250 pounds)
- Has no stitches to remove, only a Band-Aid to remove in one week.
- The patient goes home 1-2 hours after the procedure (average is 1 hour 35 min)
- No patients had to spend the night in the hospital out of the past 12,000+ operations*
- Can be performed on patients of ALL ages
- Requires the patient to take only one day off of work--the day of surgery
- Allows the patient to resume 'regular' duties the next day--no restrictions.
- Changes people's lives by curing this disease and eliminating their symptoms!
- We do mini-surgery on everybody...
- We understand that everybody can't come here, but please find the best surgeon you can.
*Note... some patients have thyroid problems which have to be addressed during their parathyroid surgery. Usually, this means a thyroid nodule has to be removed... occasionally, more of the thyroid gland has to be removed. We remove a thyroid nodule or some other portion of a thyroid gland in about 28% of all of our operations. The removal of a thyroid nodule or two usually means the operation takes about 1-10 minutes longer. These patients are treated exactly as those that do not have any surgical procedures done to their thyroid gland, and people with thyroid nodule removal go home exactly the same. In other words, removing a thyroid nodule or portion of the thyroid gland during a mini parathyroid operation simply means the operation will take a few minutes longer. NOTHING else is different. The incision is the same. The anesthesia is the same. The bandage is the same. Over 99% of these people still go home within a couple of hours. We keep 1 patient in the hospital overnight for every 500 or so parathyroid operations, and these are typically people who have a huge thyroid goiter that goes down into their chest. Remember, patient safety is absolutely priority number one. If anybody is not doing well, has problems, or needs to stay for any reason... then they should stay.
Watch our two videos of this MIRP mini-parathyroid operation.
Click Here to watch the new one filmed in August, 2011. Much less formal but shows what we have learned from doing one operation nearly 17,000 times when this was filmed. Best page on Parathyroid.com.
Click Here to watch the one filmed in 2005. This is more formal but shows more of the operation. This video was shown on national TV. Now shown on YouTube. This is the old way we did the operation where we operated on one side of the neck only.
Frequently Asked Questions About MIRP Parathyroid Surgery and Mini Parathyroid Surgery
-
What kind of anesthesia will be used for a mini-parathyroid surgery?
We use a light general anesthesia almost exclusively--this is not endotracheal general anesthesia and does not require a breathing tube down your throat (trachea), nor does a machine have to breath for you. You receive anesthetic medication in your veins and inhaled medication through the LMA, which sits in your mouth. Patients breathe for themselves, but don't feel or remember anything. They wake up within 5 minutes or so, and can be ready to leave the hospital in about 1 to 1.5 hours. -
My sestamibi scan is negative, can I still have a mini-parathyroid operation?
Most sestamibi scans are performed by radiology departments that only do a few scans per year... and their scans are terrible. Some places that do Sestamibi scans frequently have terrible (worthless!!) scans. DO NOT let the fact that you have a negative scan preclude you from having a mini-parathyroid operation! Do not let your doctor tell you that you are not a candidate for mini-parathyroid operation based upon a negative scan... it's not that simple! Virtually ALL patients with hyperparathyroidism can have a MIRP mini-parathyroid operation if your surgeon is an expert in parathyroid surgery. Dr Norman and his team of surgeons do mini operations on 100%. Over 75% of patients we operate on have a NEGATIVE scan done somewhere else before coming here. Watch the video showing how we do the SAME operation on scan negative and scan positive patients. -
What is the recovery period? When can I go back to 'normal' activities?
Patients who have a mini-parathyroid operation (a MIRP) should expect to have dinner with their families the evening of surgery, and go back to work the next day. If your surgeon tells you that you will need a week or two of recovery time from parathyroid surgery, this is a sign that he/she does not do much parathyroid surgery. If you are told this--you may want to find another surgeon who is more up to date. It is simply not true. Remember, recovery from surgery involves many factors... one is the health of the patient, but the duration of the operation, the amount of anesthesia given, the size of the wound, how much tissue is dissected inside the neck, how much tissue has to be sewn back together, etc, etc, all play a part in how patients feel after the operation. As a general rule, big operations take people longer to get over than small operations. It's true for gallbladder surgery, hernia surgery, and parathyroid surgery. -
What about stitches? Tell me about the wound.
Most surgeons who do mini-surgery of all types understand that scar size and wound care are important issues. Mini-parathyroid operations should be closed in a 'plastic' surgery type of closure with all the stitches on the inside. This has the highest chances of a nice thin scar, and the patient doesn't have to worry about having the stitches removed...they all dissolve in a few weeks when the wound is healed. The wound simply needs to be kept dry for 24 hours and then the patient can shower and even swim. We tell our patients they can shower the next morning. The bandage is only 1 inch long (or less) and 1/4 inch wide. This should be one of the things your surgeon discusses with you before the operation. -
 How big will my scar be?
How big will my scar be?
This is almost entirely dependent upon the skill of your surgeon. The size of your incision should have nothing to do with your sestamibi scan or ultrasound results. The size of the incision is slightly dependent upon the size of the patient. Here you see two pictures. The picture on the left is a woman that weighs 115 pounds. The second picture is a man that weighs 245 pounds. Both have had MIRP mini-surgery performed by Dr Norman in January 2009. The woman's scar is 3/4 inch. The man's scar is 1 inch. We use a small incision on 100% of patients, even those with a negative scan. Did you see the size of the scar when a surgeon does the "exploration" surgical method? -
Do you have information written BY PATIENTS who have had mini-surgery?
Most patients feel alone when they are told they have parathyroid disease. They have never heard of parathyroid glands, don't know what they do, and don't know anybody else that has had a parathyroid gland problem. Click here to read about people just like you who have undergone a MIRP mini-parathyroid operation. -
Do you have pictures of parathyroid adenomas (parathyroid tumors) removed from patients with hyperparathyroidism? Yep, click here to see lots of pictures.
What to read next
- Watch the movie of a 13-minute, 4-gland parathyroid operation. This is state of the art and this is absolutely the most informative page of this website.
- If you like learning by watching videos, then go to our Video Page to watch short videos on most parathyroid topics.
- More on Minimally Invasive Radioguided Parathyroidectomy (why it was developed).
- Look at a sampling of parathyroid tumors removed from patients with hyperparathyroidism. Look at these tumors and compare your calcium and PTH levels to other patients like yours. New
- More about Dr. Norman and the Norman Parathyroid Center.
- How to become our patient.
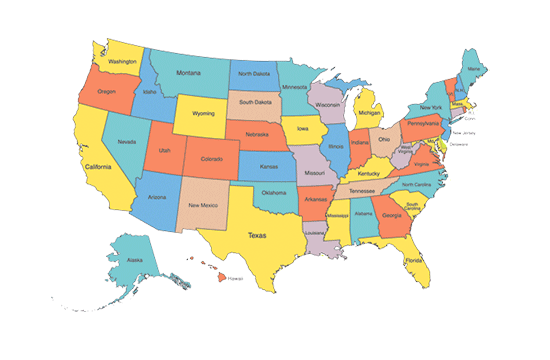
- See a map of where our patients come from. People love the map!