Interesting Parathyroid Cases
Interesting case of the week 7/1/2022 with Dr. Luke Watkins
Interesting case of the week 6/24/2022 with Dr. Luke Watkins
Interesting case of the week 6/17/2022 with Dr. Luke Watkins
Interesting case of the week 6/10/2022: Even people with small tumors or relatively low levels can have big symptoms, with Dr. Luke Watkins

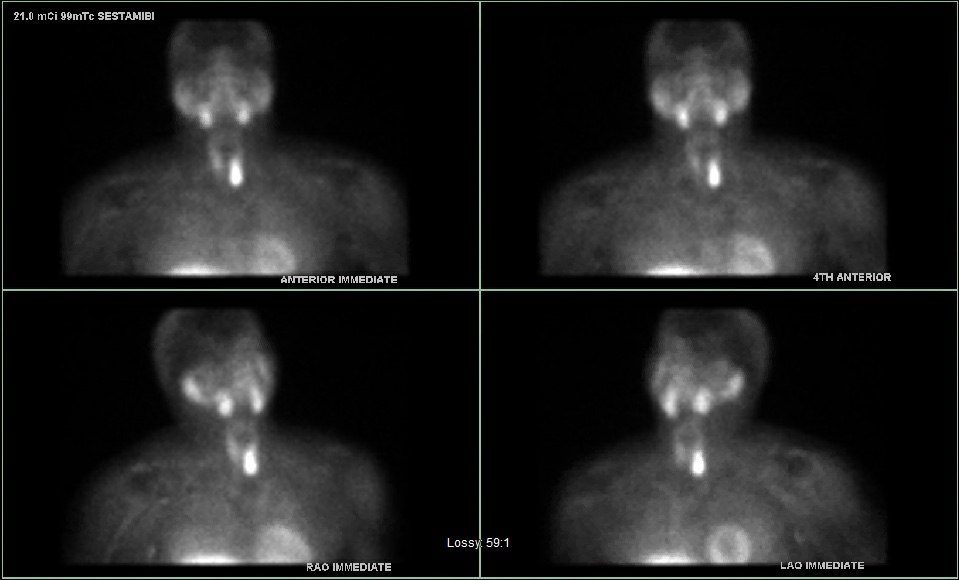
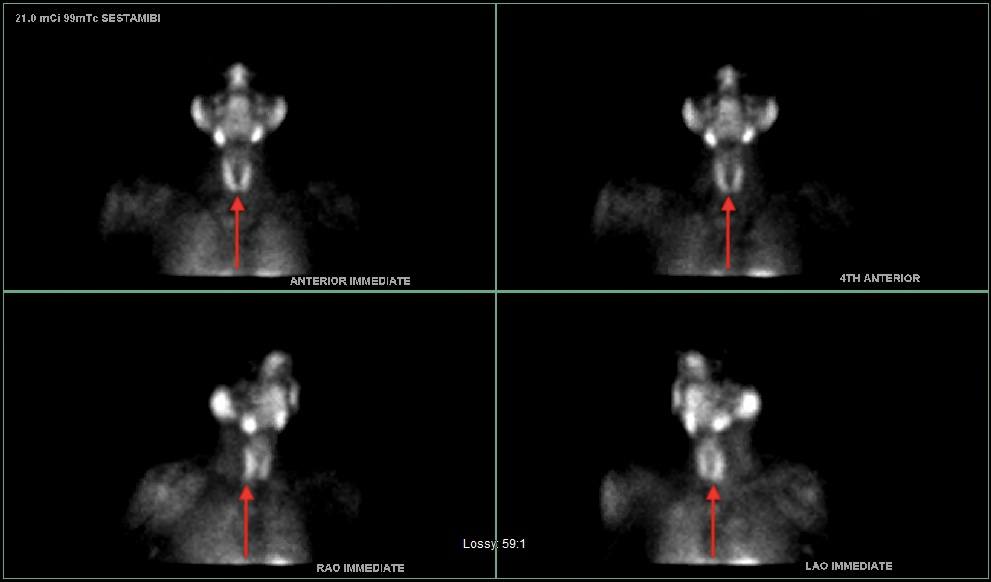
Interesting case of the week 6/3/2022: Parathyroid Tumor DEEP in the Chest with Dr. Drew Rhodes
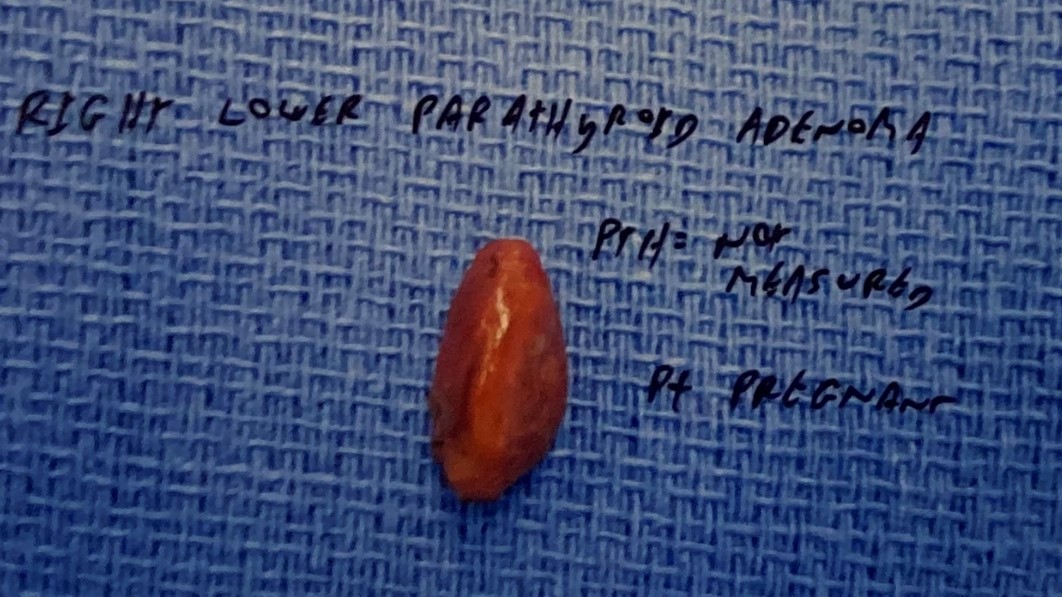
Interesting case of the week 5/27/2022: The Norman-Way in Pregnancy with Dr. Drew Rhodes
Interesting case of the week 5/20/2022 with Dr. Luke Watkins
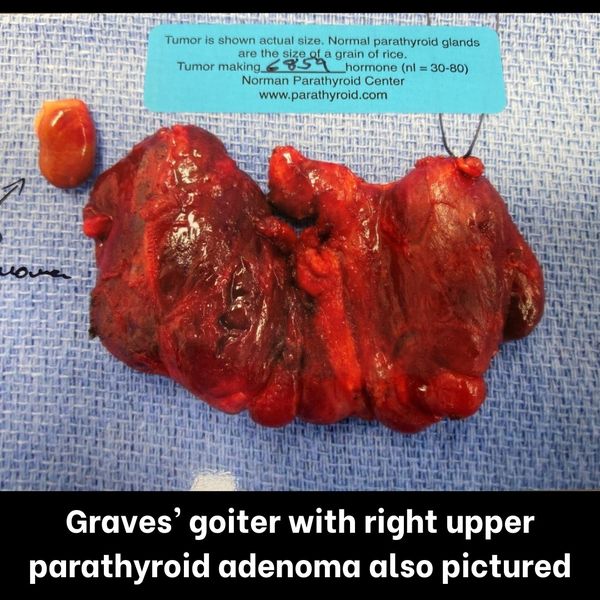
Interesting case of the week 5/13/2022: Two Birds, One Surgery with Dr. Drew Rhodes
Interesting case of the week 5/6/2022: Importance of the Norman-Way in Finding YOUR Tumor with Dr. Drew Rhodes
Interesting case of the week 4/29/2022 with Dr. Luke Watkins
Interesting case of the week 4/22/2022 with Dr. Luke Watkins
Interesting case of the week 4/15/2022 with Dr. Luke Watkins
Interesting case of the week 4/8/2022 with Dr. Luke Watkins
Interesting case of the week 4/1/2022: Two hormonal dysfunctions, one patient with Dr. Drew Rhodes
Interesting Case of the Week 3/25/22 with Dr. Luke Watkins
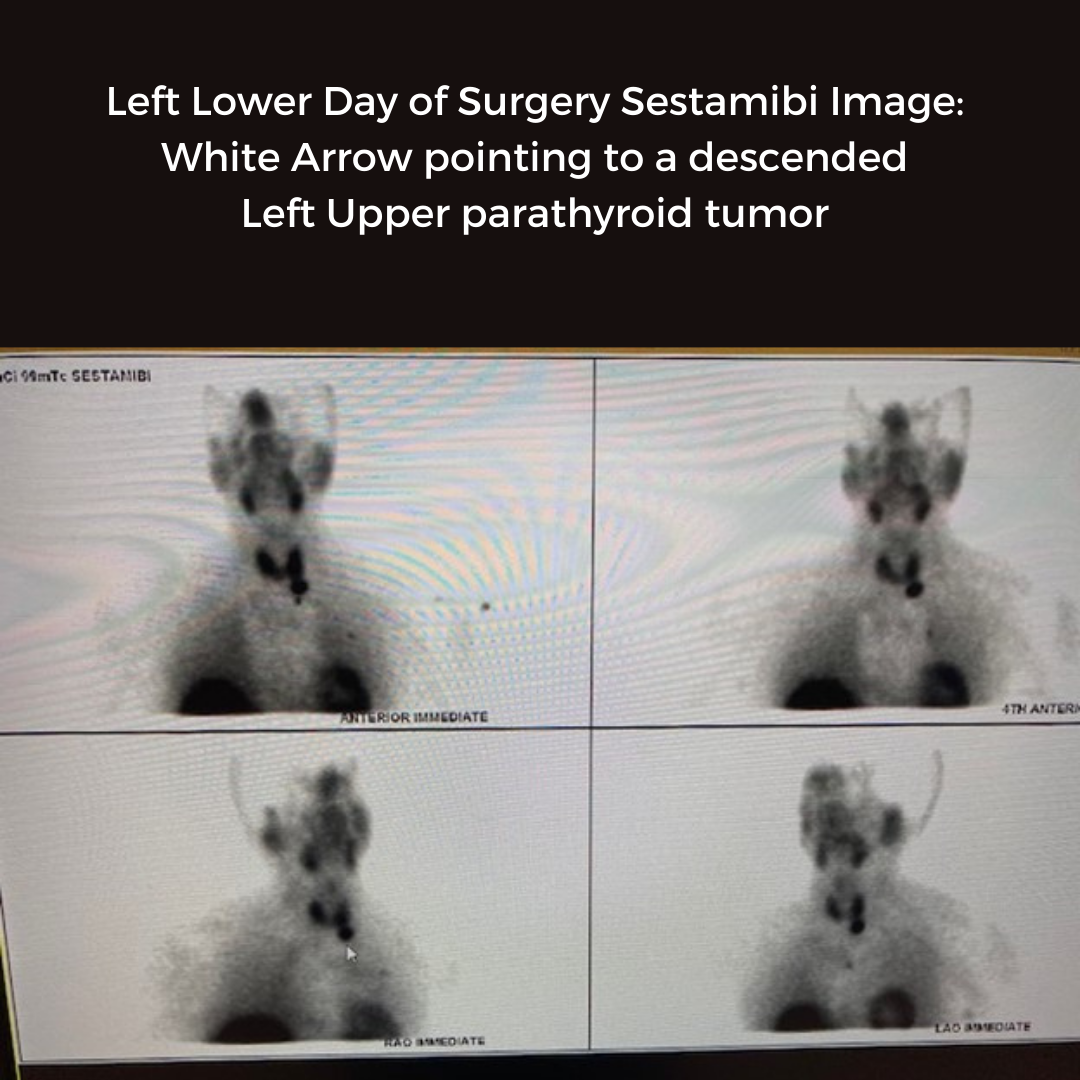
Interesting Case of the Week 3/18/22: Misleading preoperative imaging with Dr. Drew Rhodes
Interesting case of the week 3/11/22 with Dr. Kevin Parrack
Interesting case of the week 3/4/22 with Dr. Luke Watkins

Interesting case of the week 2/25/22 with Dr. Luke Watkins
Interesting case of the week 2/18/22: Modest PTH can be hiding monster tumors, with Dr. Drew Rhodes
Interesting case of the week 2/11/22 with Dr. Luke Watkins

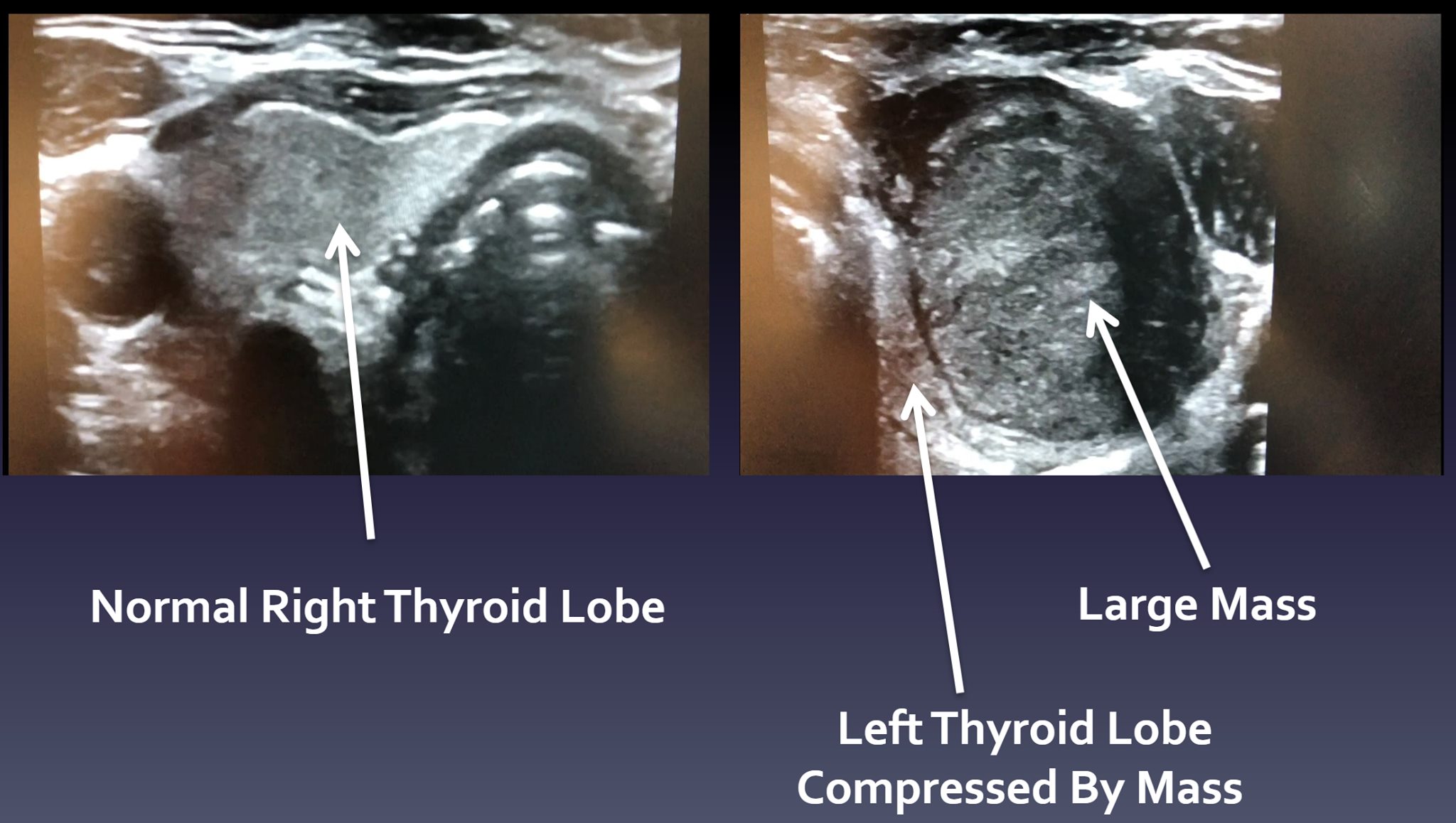
Interesting Case of the Week 2/4/22: Patients with modest parathyroid hormone levels can have large parathyroid tumors
Interesting case of the week 1/28/22 with Dr. Kevin Parrack
Interesting case of the week 1/21/22: 25 years of high calcium with Dr. Luke Watkins
Interesting Case of the Week 1/14/22: Another case against focused parathyroidectomy with Dr. Drew Rhodes
Interesting Case of the Week 1/7/22 with Dr. Luke Watkins
Interesting Case of the Week 12/17/21: Intra-thyroidal Parathyroid Adenoma with Dr. Jamie Mitchell
Interesting case of the week 12/10/21: The importance of looking at all four glands with Dr. Luke Watkins

Interesting case of the week 12/3/21: Persistent hyperparathyroidism after surgery with intraoperative PTH monitoring with Dr. Dan Ruan
Interesting case of the week 11/19/21: Recognizing Non-Classic Lab Values in Patients with Primary Hyperparathyroidism with Dr. Jamie Mitchell
Interesting case of the week 11/12/19 with Dr. Luke Watkins

Interesting case of the week 11/5/21 with Dr. Kevin Parrack

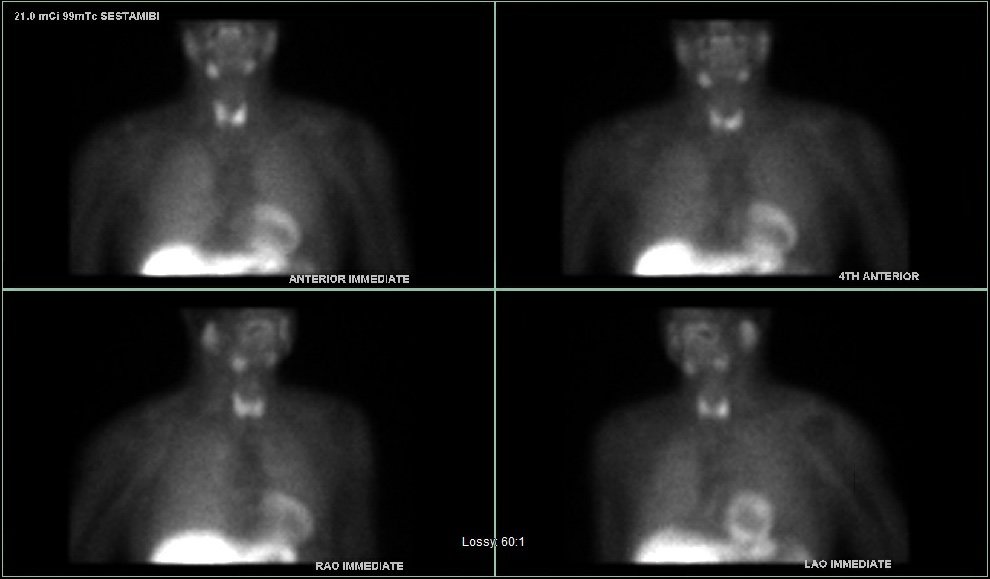
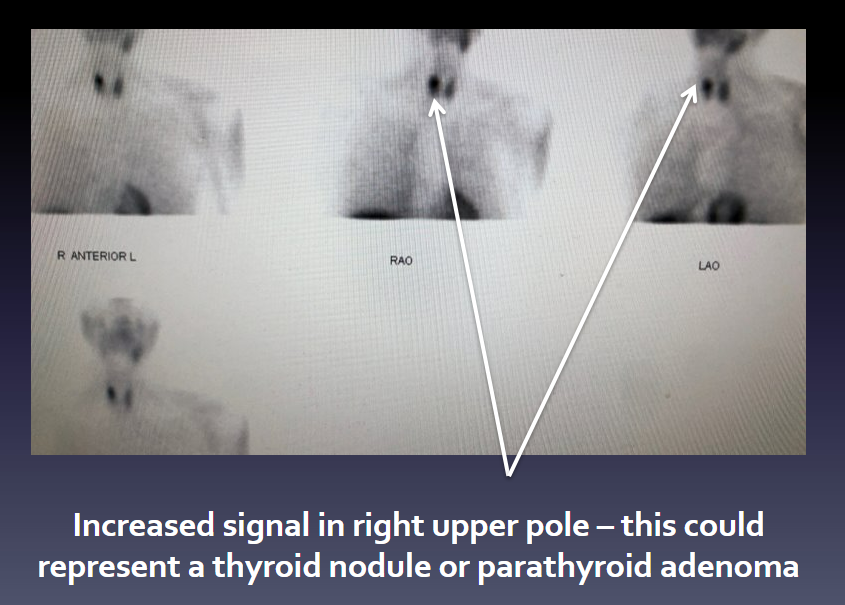
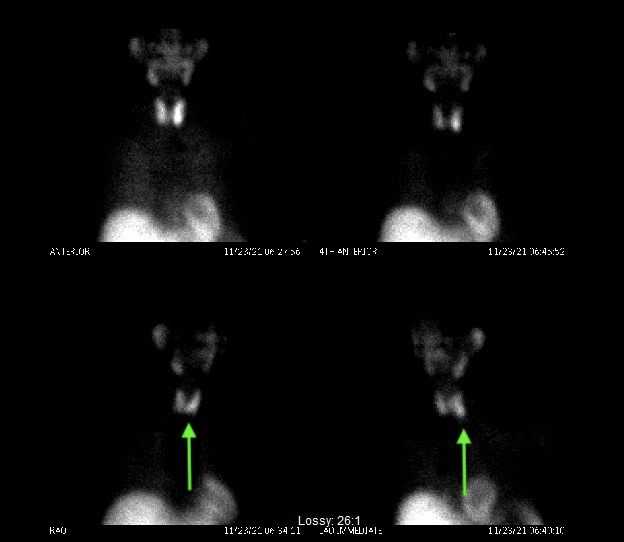
Interesting case of the week 10/22/21: Abnormally normal PTH with Dr. Drew Rhodes
This week, we saw a recently retired biochemist and officer with the Air Force. During our initial visit, he told me he could barely get out of bed anymore due to debilitating pain.
Keep in mind this guy is a former US Air Force officer and triathlete. He is not used to having his butt kicked by anything, let alone hyperparathyroidism.
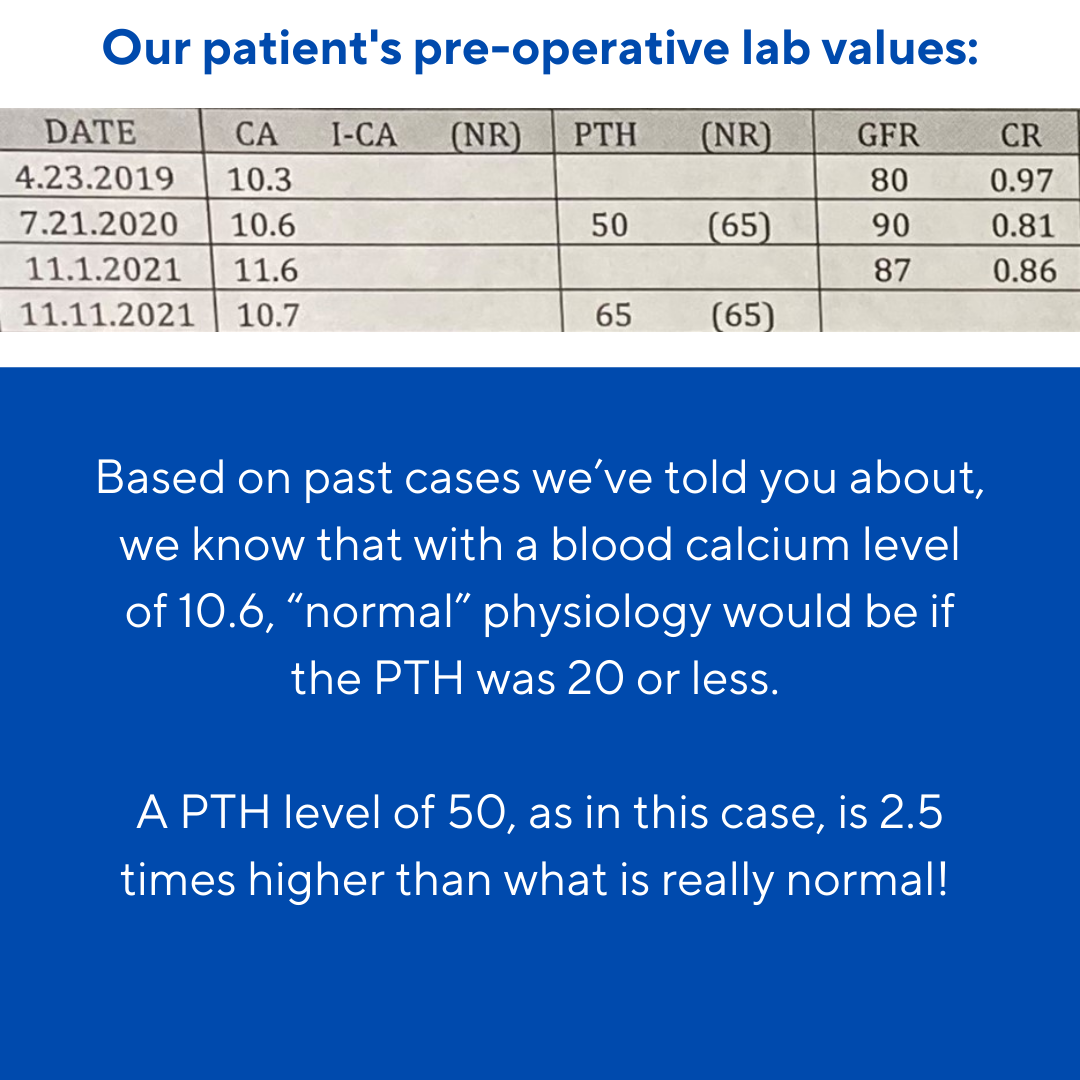
Preoperatively, his PTH was in the 50s, but his calcium levels were 10.5 and 10.7.
In roughly 20% of our patients, we see this phenomenon of "abnormally normal PTH" levels. This phenomenon can cause patients to suffer longer than necessary, since many providers will wait for the PTH level to increase above the "normal" range before recognizing their patient is suffering with primary hyperparathyroidism.
Meanwhile, the disease is wreaking havoc on the patient's body.
From our collective experience of over 60,000 cases, we know that it doesn't matter if your PTH is 50 or 150 – but it does matter what your PTH is doing in relation to your calcium level. And when your calcium level is 10.5, your PTH should be less than 20. The purpose of the parathyroid glands is to regulate the blood calcium level and recognize that when the calcium level is that high, PTH does not need to be released into the system to pull more calcium from the bones into the bloodstream.
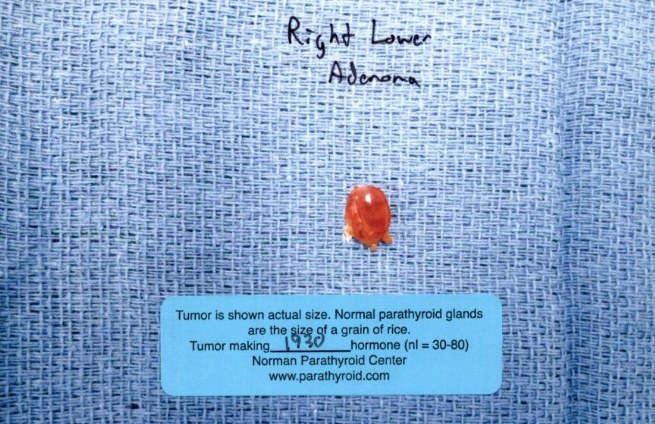
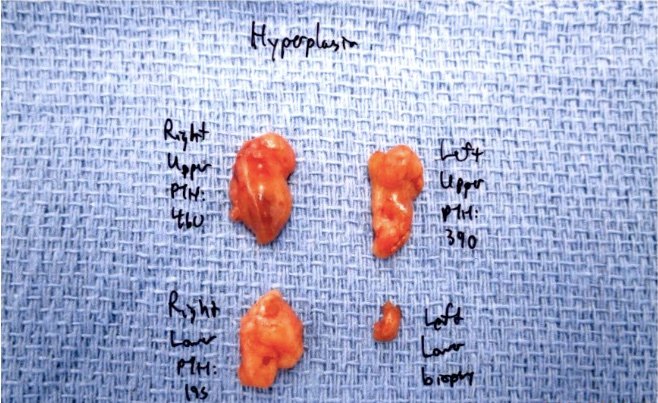
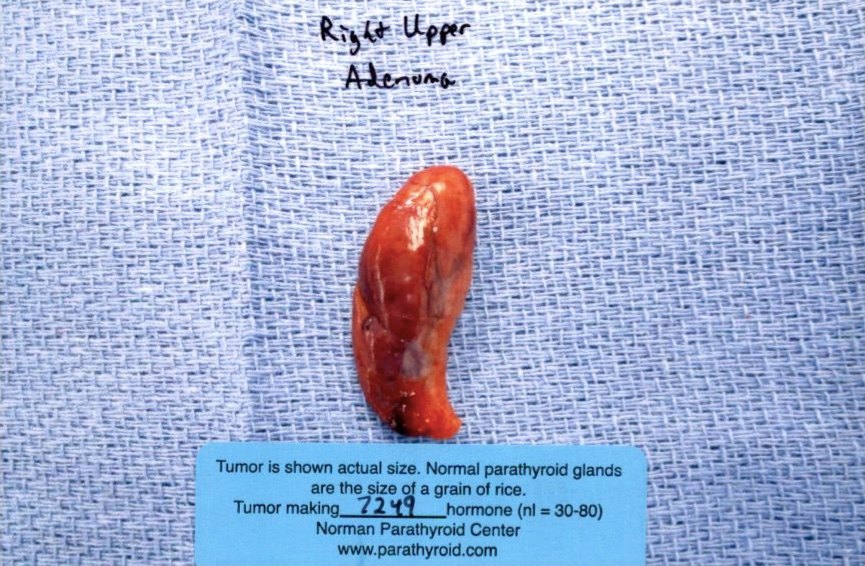
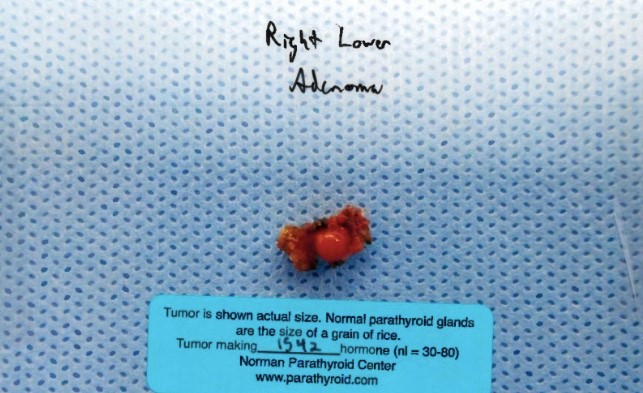
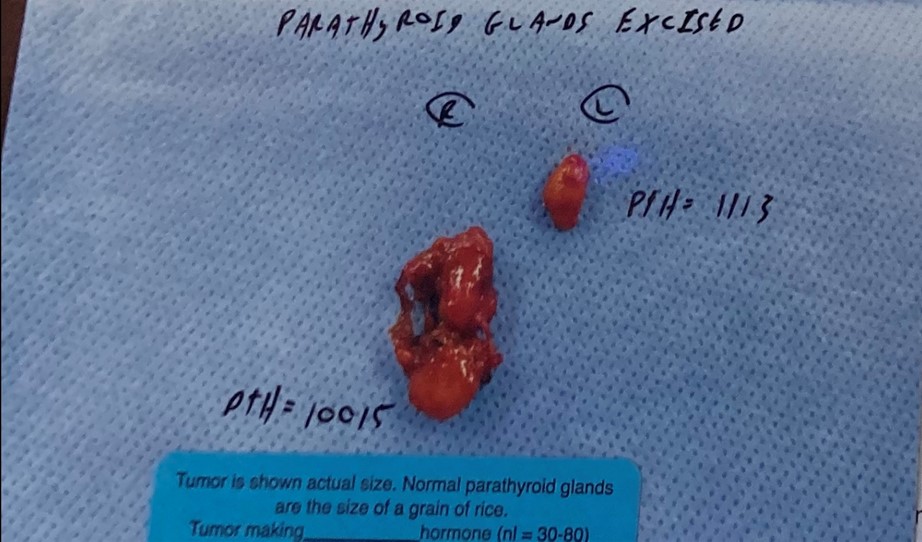
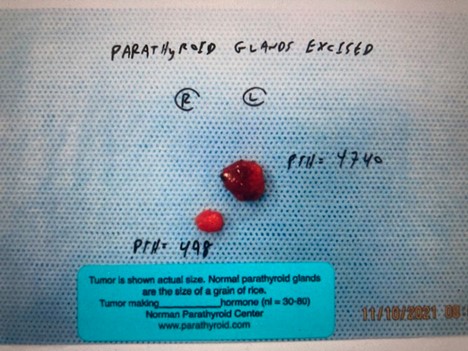
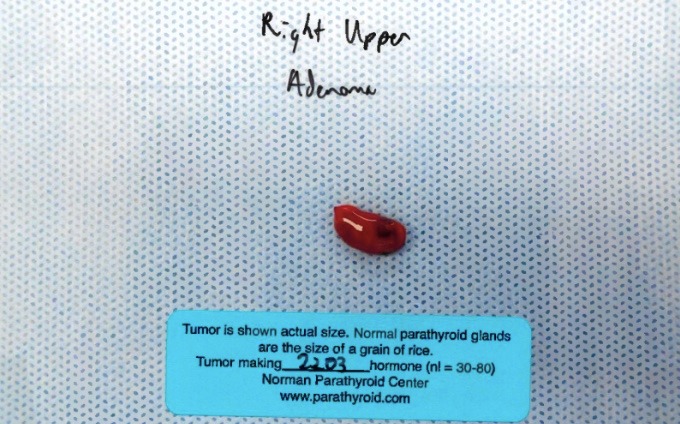
Intraoperatively, two parathyroid tumors were found. Normal parathyroid gland intraoperative PTH production is roughly 50 units, with his tumors producing 333 and 2267 units. His post-operative blood PTH was 15. This is a great example of a patient with "normal" pre-op PTH levels being cured with surgery.
The evening before his surgery, he told me he had been unable to figure out a math problem for his current coursework toward another graduate degree. On the night of surgery, the problem made sense! Just three days after surgery, he sent me a picture of him crossing the finish line at his first race in years. He said it was his "couch to 5K" miracle.
We know there was no miracle, but rather good surgery allowing him to feel whole again.
Interesting case of the week 10/15/2: Another parathyroid gland trying, and failing, to hide with Dr. Luke Watkins
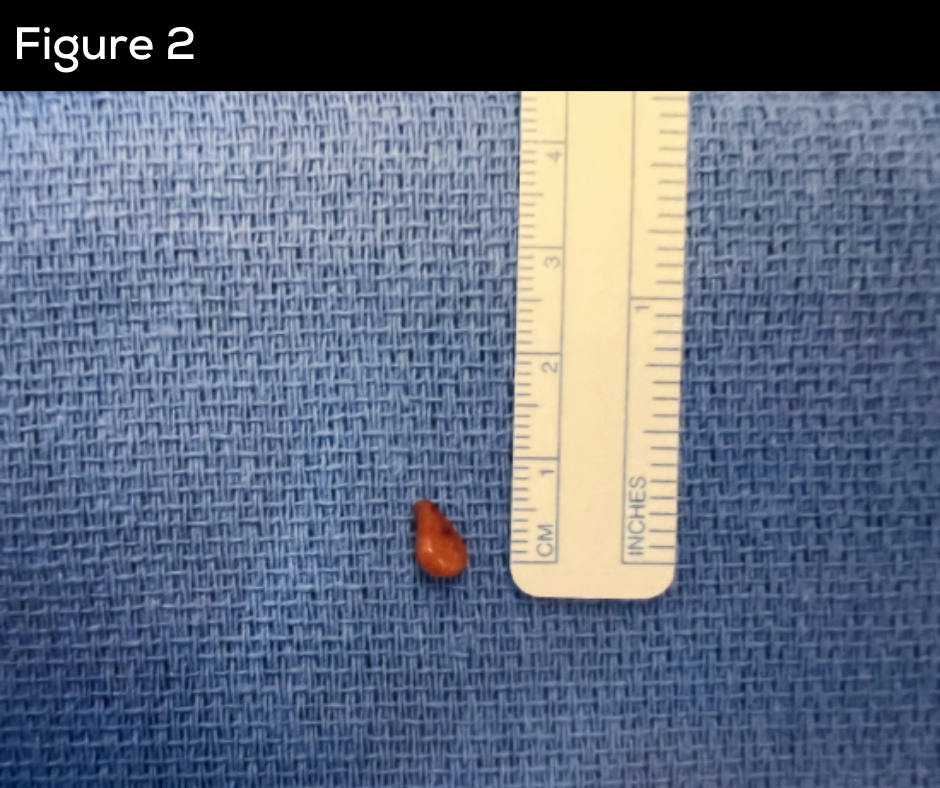
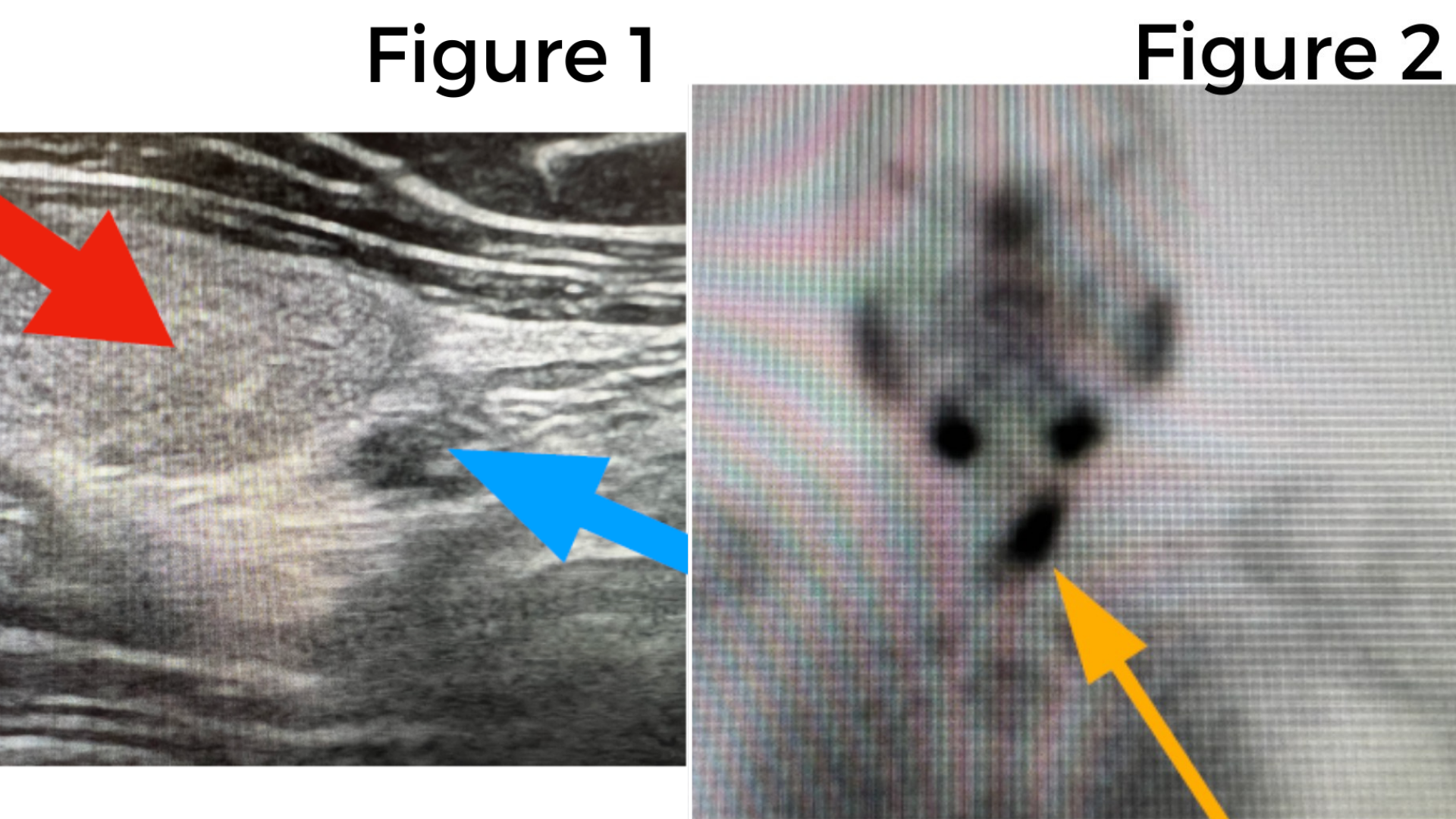
This week we're discussing a 56-year-old female who travelled across the country to see us for her parathyroid surgery. Her calcium level was 10.6 with a PTH of 81, clearly demonstrating primary hyperparathyroidism.
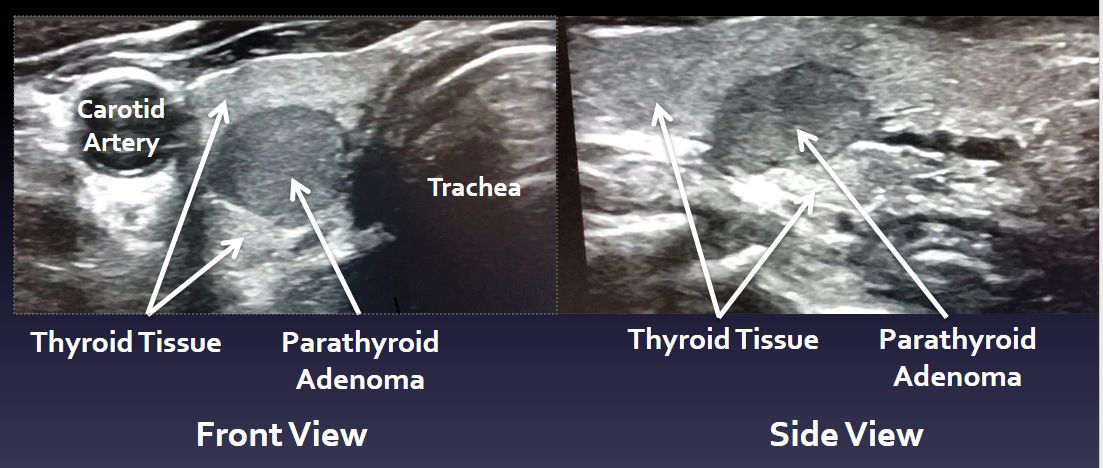
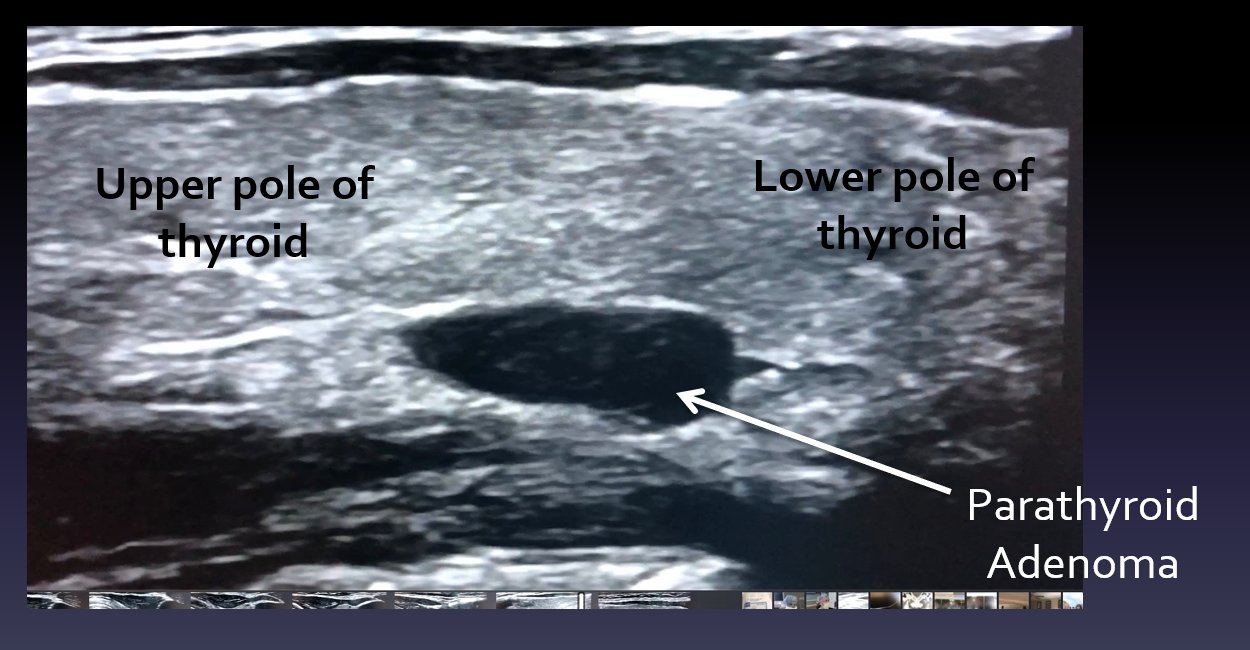
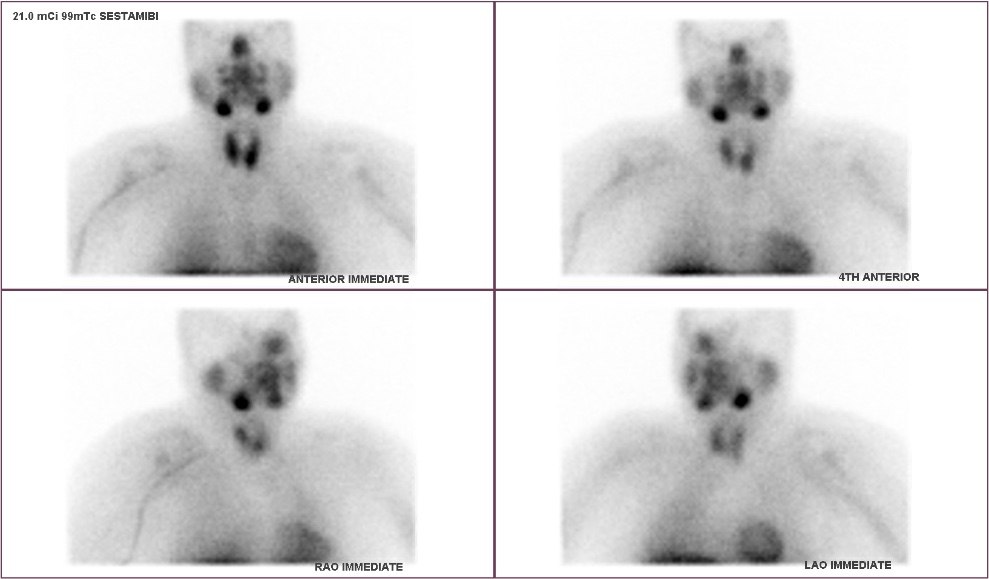
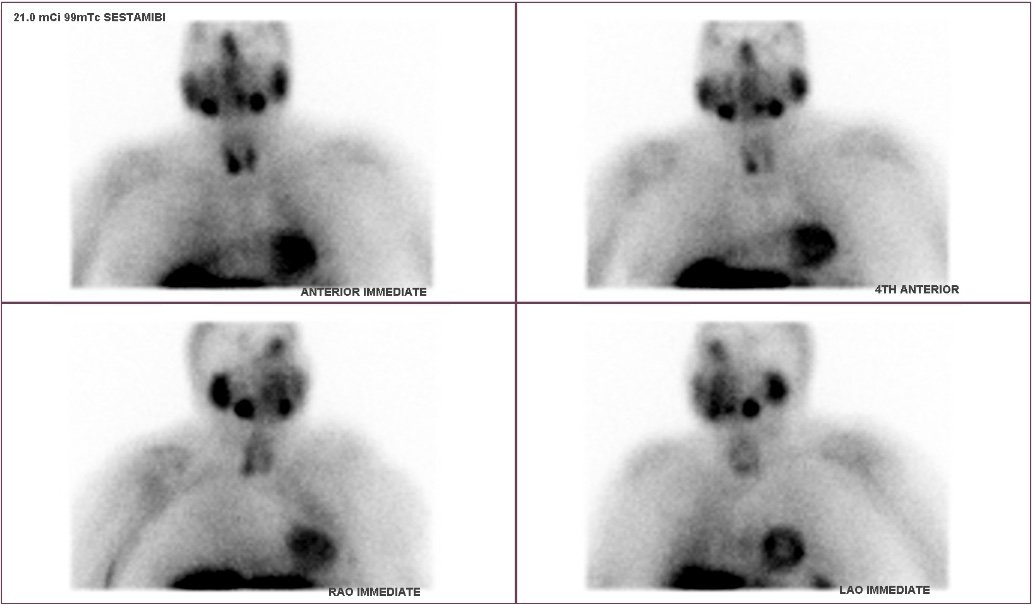
She had been taking lithium, which can cause hyperparathyroidism, and had worsening kidney function. She also had multiple symptoms, including fatigue, insomnia, irritability, and brain fog. Prior to being sent to us, she had a sestamibi scan and an ultrasound that did not note any parathyroid glands.
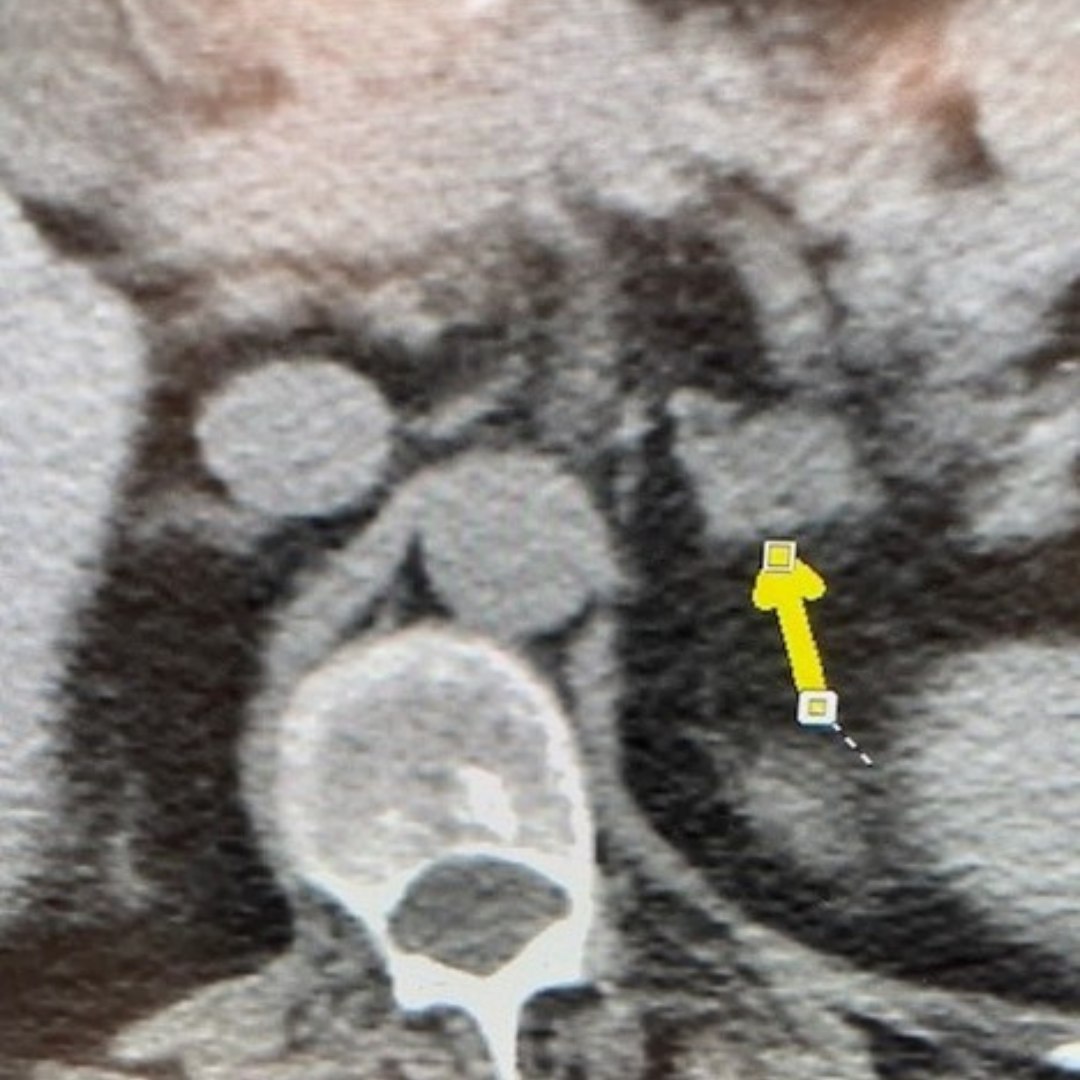
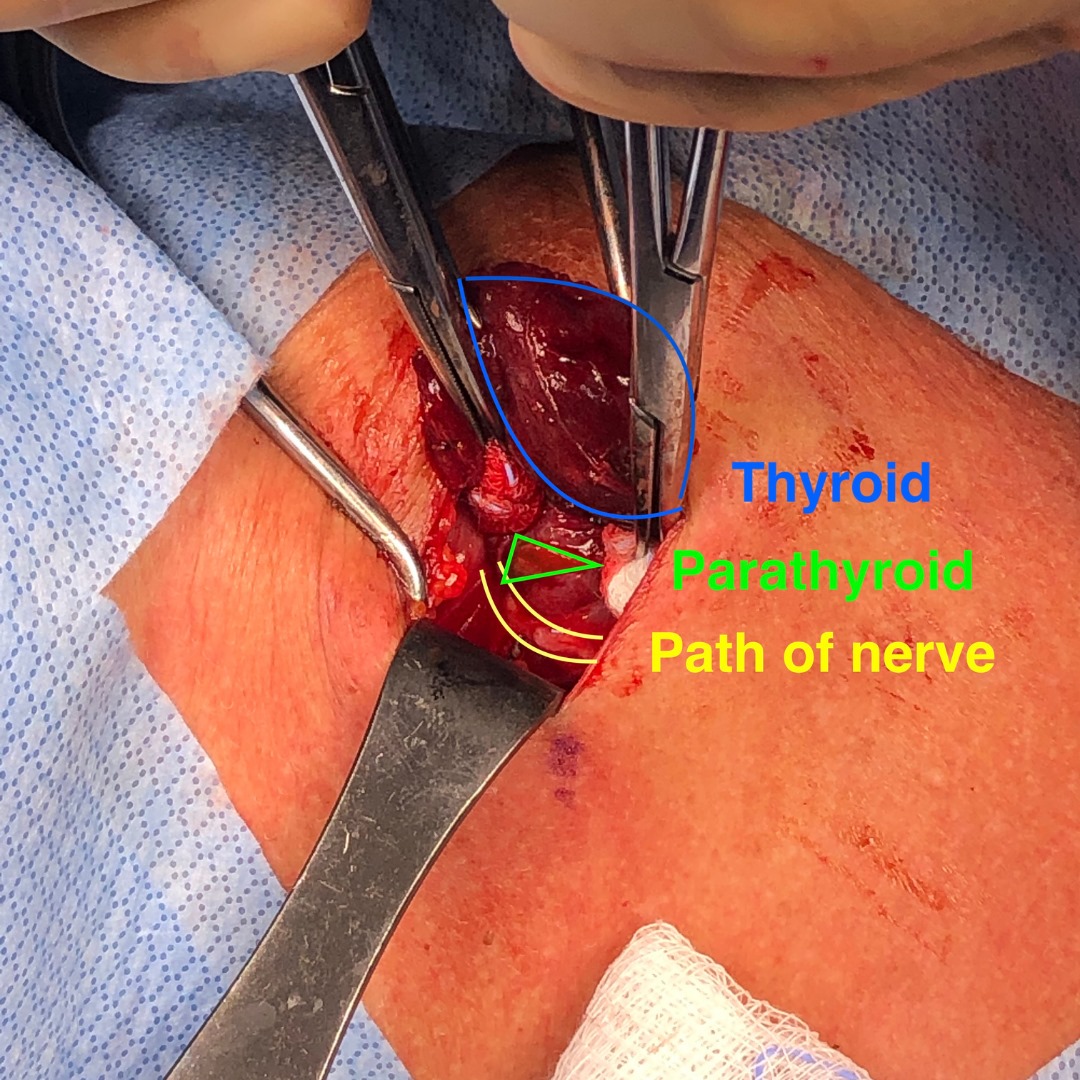
During her surgery, we quickly found three mildly enlarged, or hyperplastic, parathyroid glands. One gland was not in any of the usual places. But we know where these glands like to hide. After checking the more common locations, we separated part of the thyroid gland from its blood supply to fold the upper part down and look behind it. Her fourth gland was hiding between the thyroid and the windpipe, just millimeters away from the nerve for her voice.
Our knowledge of parathyroid anatomy and experience helped us find this gland, which was over-functioning. Without finding it, she would not have been cured.
The image below was taken at the time of surgery and is marked to show the thyroid gland being retracted in blue, the path to the nerve to the vocal cords between the yellow lines, and the parathyroid gland in the green triangle.
Interesting case of the week 10/8/21: Parathyroid Carcinoma Presenting As Recurrent Primary Hyperparathyroidism with Dr. Jamie Mitchell