Hyperparathyroidism vs Hyperthyroidism

Hyperparathyroidism vs Hyperthyroidism
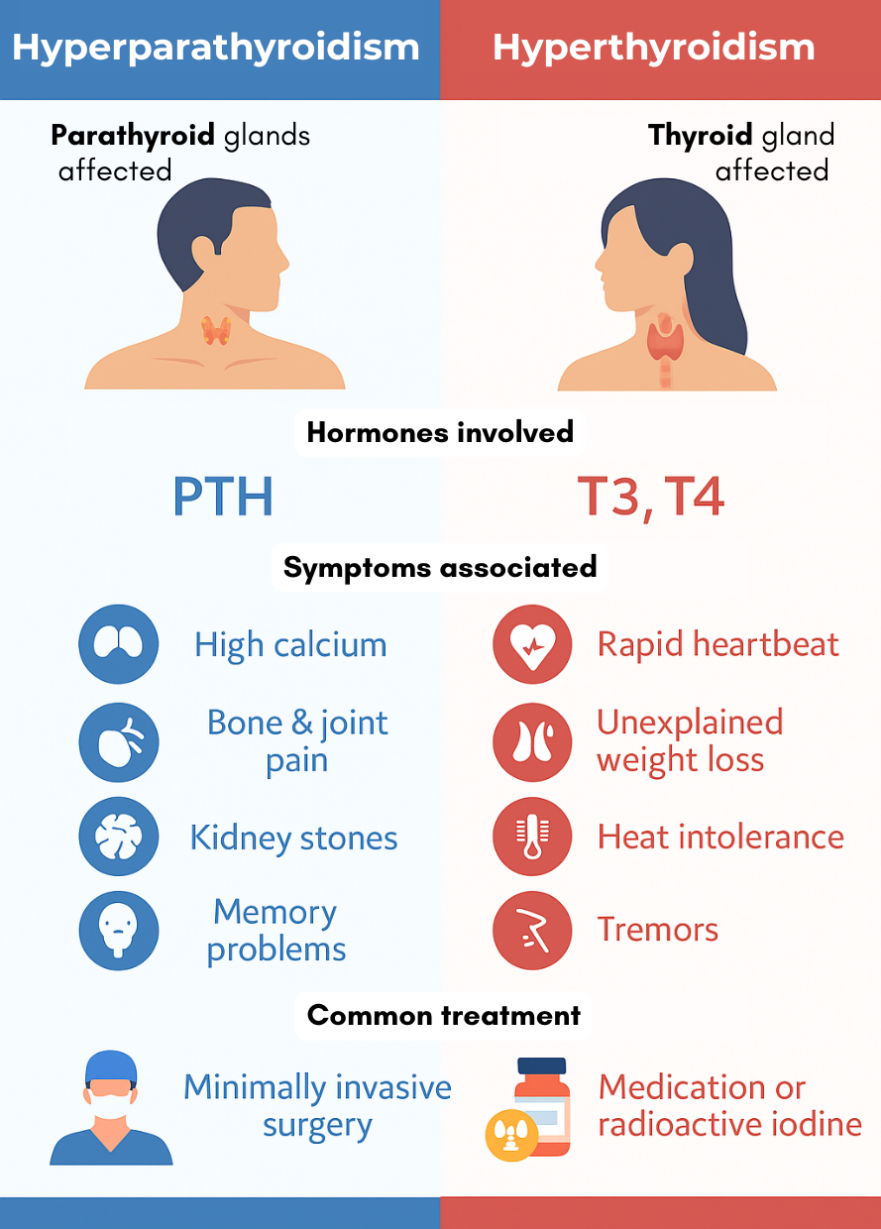
Although the names sound alike, hyperparathyroidism vs hyperthyroidism are diagnosed using very different lab tests and clinical findings, because they affect entirely separate glands and systems in the body. Hyperparathyroidism involves the parathyroid glands, leading to elevated calcium levels due to increased parathyroid hormone (PTH) secretion. In contrast, hyperthyroidism affects the thyroid gland, resulting in elevated levels of thyroid hormones (T3 and T4) and suppressed TSH. Understanding these distinct diagnostic markers is essential for avoiding misdiagnosis and ensuring patients receive the correct treatment.
Hyperparathyroidism Diagnosis
Hyperparathyroidism is diagnosed with the following:
- Calcium levels: High calcium is the key indicator.
- Parathyroid hormone (PTH): PTH is elevated or inappropriately normal despite high calcium.
- Vitamin D: Often low or borderline low.
- Bone density scans and kidney function tests may also be used to assess complications.
Importantly, blood calcium must be measured multiple times over months or years. Many patients have had high calcium for years without being diagnosed.
Hyperthyroidism Diagnosis
Hyperthyroidism is typically diagnosed with:
- TSH (thyroid-stimulating hormone): Suppressed or low
- Free T3 and Free T4: Elevated
- Thyroid antibodies: Can help diagnose autoimmune causes like Graves’ disease
- Thyroid ultrasound or radioactive iodine uptake scan: May be used to evaluate nodules or thyroid function
This testing approach is entirely different from what’s required for hyperparathyroidism, emphasizing how distinct these conditions truly are.
Hyperparathyroidism vs Hyperthyroidism: Treatment
Although the names sound alike, hyperparathyroidism vs hyperthyroidism are diagnosed using very different lab tests and clinical findings, because they affect entirely separate glands and systems in the body. Hyperparathyroidism involves the parathyroid glands and leads to elevated calcium due to increased parathyroid hormone (PTH). In contrast, hyperthyroidism affects the thyroid gland and results in elevated thyroid hormones (T3 and T4), with a suppressed TSH. Understanding these distinct diagnostic markers is essential for avoiding misdiagnosis and ensuring patients receive the correct treatment.
Hyperparathyroidism Treatment
Surgery is the only cure for primary hyperparathyroidism. In over 95% of cases, the disease is caused by a single benign parathyroid tumor (adenoma), which can be removed with a minimally invasive operation. In about 30% of cases, two or more glands are affected.
Medical management of hyperparathyroidism is not curative and is not recommended in most patients. The longer high calcium levels persist, the greater the risk of complications such as osteoporosis, kidney stones, and cardiovascular issues.
Hyperthyroidism Treatment
Hyperthyroidism can be treated with:
- Antithyroid medications (like methimazole)
- Radioactive iodine therapy to shrink or destroy the thyroid
- Surgery to remove the thyroid gland in some cases
Unlike hyperparathyroidism, medications are often the first line of treatment in hyperthyroidism, particularly in cases of Graves’ disease.
Hyperparathyroidism vs Hyperthyroidism: Why the Confusion?
The confusion between hyperparathyroidism vs hyperthyroidism is understandable. The names are similar, both conditions involve neck glands, and both can affect energy levels and mood. However, failing to distinguish the two can lead to delays in proper diagnosis and treatment.
Patients with hyperparathyroidism are frequently misdiagnosed with depression, chronic fatigue syndrome, or even hyperthyroidism—especially if their calcium levels are only mildly elevated or they “look fine on paper.”
If you’ve been told your calcium is high or your PTH is elevated, don’t assume it’s a thyroid issue. Make sure you see an expert who can evaluate your parathyroid glands and help determine if surgery is necessary.
Hyperparathyroidism vs Hyperthyroidism: The Bottom Line
When comparing hyperparathyroidism vs hyperthyroidism, it’s clear that these are two very different conditions with unique causes, symptoms, diagnostics, and treatments. The key differences can be summarized as:
- Affected gland: Parathyroid vs Thyroid
- Hormone involved: PTH vs T3/T4
- Main effect: High calcium vs High metabolism
- Symptoms: Fatigue, bone pain, kidney stones vs Rapid heartbeat, weight loss, heat intolerance
- Treatment: Surgery (hyperparathyroidism) vs Medication or radioiodine (hyperthyroidism)
If you or someone you know is experiencing symptoms that could relate to either of these conditions, make sure to get the correct tests and see a specialist familiar with hyperparathyroidism vs hyperthyroidism. A proper diagnosis can change your life—and in the case of hyperparathyroidism, surgery can be curative in almost every case.
Additional Resources:
- Learn more about the Norman Parathyroid Center.
- Read more on the Parathyroid blog.
- Become our patient.
- Check out our sister surgeons at the Clayman Thyroid Center, and the Carling Adrenal Center. We are now united under one roof, operating at the Hospital for Endocrine Surgery.