Understanding Parathyroid Adenoma and Parathyroid Nodules: What You Need to Know

Understanding Parathyroid Adenoma and Parathyroid Nodules: What You Need to Know
What Is a Parathyroid Adenoma?
A parathyroid adenoma is a benign tumor on one of the four parathyroid glands located in your neck. These tiny glands—each about the size of a grain of rice—play a critical role in regulating calcium levels in your body through the production of parathyroid hormone (PTH). When a parathyroid adenoma develops, it begins to produce too much PTH, leading to a condition called primary hyperparathyroidism.
While the word “tumor” may sound alarming, a parathyroid adenoma is not cancer. It is a non-cancerous growth that can, however, have serious health consequences if left untreated. This includes osteoporosis, kidney stones, high blood pressure, fatigue, memory problems, and more.
What Is a Parathyroid Nodule?
Many patients confuse parathyroid nodules with thyroid nodules, but they are not the same. A parathyroid nodule is often another term used when a parathyroid gland appears enlarged or irregular on imaging. In most cases, a parathyroid nodule is a parathyroid adenoma. While the term “nodule” is sometimes used interchangeably, it’s important to understand the underlying cause because treatment is different.
If you’ve been told you have a parathyroid nodule, you should be evaluated by an experienced parathyroid expert to determine whether it’s functioning normally or producing excess hormone.
Parathyroid Adenoma vs. Thyroid Nodule
It’s very common for imaging to mistakenly identify a parathyroid adenoma as a thyroid nodule, especially if the radiologist or physician isn’t highly experienced with endocrine imaging. Parathyroid glands sit just behind or next to the thyroid gland, so a parathyroid nodule can easily be confused with a thyroid abnormality.
But there’s a big difference: a thyroid nodule is not usually hormonally active, while a parathyroid adenoma actively causes damage by raising calcium levels and PTH levels in your blood. That’s why identifying and treating parathyroid adenomas properly is critical.
What Causes a Parathyroid Adenoma?
A parathyroid adenoma typically occurs when one of the four parathyroid glands grows out of control and begins secreting too much parathyroid hormone. This overproduction of PTH causes calcium to be pulled from the bones into the bloodstream, leading to elevated calcium levels.
The exact cause of a parathyroid adenoma is often unknown. In rare cases, it may be associated with inherited conditions, such as MEN-1 (Multiple Endocrine Neoplasia). However, most cases occur sporadically and are more common in women over 50.
Symptoms of a Parathyroid Adenoma
Because the symptoms of parathyroid adenoma are often vague or attributed to aging, the condition is frequently missed or misdiagnosed. Some of the most common signs include:
- Fatigue
- Bone pain or osteoporosis
- Kidney stones
- Memory loss or brain fog
- Depression or anxiety
- Muscle weakness
- High blood pressure
- Gastrointestinal issues
If you have elevated calcium and PTH levels and any of these symptoms, a parathyroid adenoma should be strongly considered.
Diagnosing a Parathyroid Adenoma
The diagnosis of a parathyroid adenoma is based primarily on laboratory testing and high-resolution imaging. Key tests include:
- Serum calcium (typically high)
- Parathyroid hormone (PTH) (also elevated)
- 24-hour urine calcium (to rule out other causes)
- DEXA scan (to assess bone loss)
Imaging is often performed using high-resolution ultrasound, 4D-CT, and Sestamibi scans. At the Norman Parathyroid Center, we specialize in accurately locating parathyroid adenomas—even those missed by other facilities.
Why “Waiting and Monitoring” Doesn’t Work
Many physicians recommend a "watch and wait" approach for patients with a suspected parathyroid adenoma, especially if their calcium levels are only mildly elevated. This is a mistake.
A parathyroid adenoma will not go away on its own. Over time, it will continue to cause bone loss, increase the risk of kidney stones, and impact cognitive and emotional health. The damage is real, and the cure is surgery.
Treatment: Surgery Is the Only Cure
The only cure for a parathyroid adenoma is surgical removal of the overactive gland. This outpatient surgery has a cure rate of over 99% when performed by an experienced, high-volume parathyroid surgeon.
At the Norman Parathyroid Center, we perform more parathyroid adenoma surgeries than any other center worldwide. Our focused approach, advanced imaging techniques, and ability to confirm cure during surgery lead to outstanding outcomes.
Why Experience Matters
Surgery for parathyroid adenomas requires expert knowledge of parathyroid anatomy and imaging. The average ENT or general surgeon performs just a few of these surgeries a year. Our surgeons perform over 4,000 parathyroid operations annually.
This matters because parathyroid glands are small, variable in location, and can be easily missed. Inexperienced surgeons may fail to find the parathyroid adenoma, or worse, may remove the wrong tissue.
What to Expect During Surgery
At our center, most patients undergo a minimally invasive parathyroidectomy through a small incision. The surgery typically takes less than 20 minutes, and patients go home the same day.
Using advanced intraoperative monitoring and rapid hormone testing, we confirm that the parathyroid adenoma has been removed and PTH levels have normalized before the patient even leaves the OR.
What Happens After Surgery?
After your parathyroid adenoma is removed, most symptoms begin to improve quickly. Many patients report better sleep, clearer thinking, less fatigue, and a general sense of well-being—often within days.
Bone health begins to recover as well, with DEXA scans showing marked improvement within 6–12 months. Calcium and PTH levels return to normal, and long-term complications are prevented.
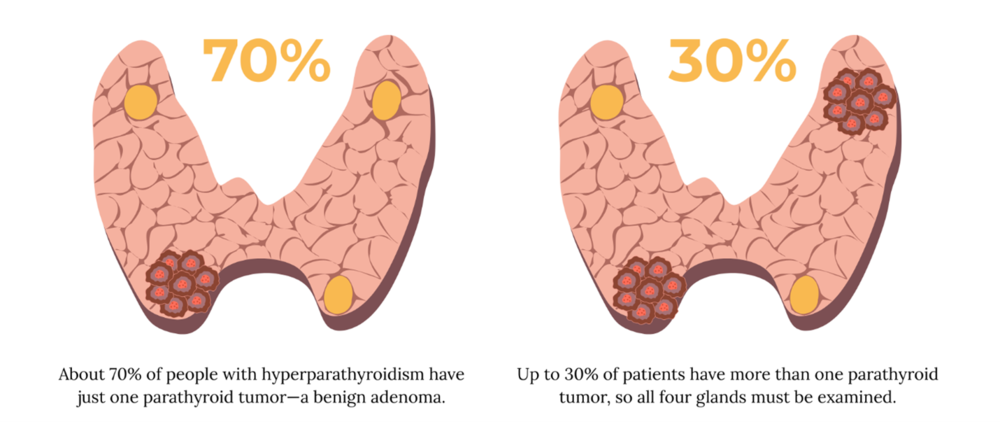
Can I Have More Than One Parathyroid Adenoma?
About 70% of people with primary hyperparathyroidism have a single parathyroid adenoma. However, about 30% of patients may have double adenomas or hyperplasia (all four glands are abnormal).
This is another reason why expert surgery is essential. Our team explores all four glands during surgery to ensure the correct diagnosis and cure. We don’t take shortcuts—and that means fewer failed surgeries and better long-term results.
What If Imaging Doesn’t Show an Adenoma?
This is more common than you think. Even in expert hands, imaging doesn’t always reveal a parathyroid adenoma—especially if it’s small, hidden, or deep in the neck or chest.
But imaging isn’t everything. If your labs suggest a parathyroid adenoma, and you have symptoms or complications, you still need surgery. Our team uses a combination of imaging, labs, and surgical experience to ensure your adenoma is found and removed.
Summary: Parathyroid Adenoma and Parathyroid Nodule
- A parathyroid adenoma is a non-cancerous tumor causing excess PTH and high calcium.
- The term parathyroid nodule is often used interchangeably, but requires expert evaluation.
- Symptoms are often vague but can be serious if left untreated.
- Surgery is the only cure and should be performed by a high-volume specialist.
- The Norman Parathyroid Center is the global leader in parathyroid adenoma treatment.
Ready to Get Answers?
If you've been told you have a parathyroid adenoma or parathyroid nodule, or if your calcium and PTH levels are abnormal, contact the Norman Parathyroid Center today. You deserve expert care, fast answers, and a real cure.
Additional Resources:
- Learn more about the Norman Parathyroid Center.
- Read more on the Parathyroid blog.
- Become our patient.
- Check out our sister surgeons at the Clayman Thyroid Center, and the Carling Adrenal Center. We are now united under one roof, operating at the Hospital for Endocrine Surgery.